Retinal detachment surgery
If you experience retinal detachment, scheduling treatment as soon as possible is critical to minimizing your risk of vision loss. The only form of treatment for a detached retina is surgery.
Retinal detachment surgery is performed using one of three methods. A patient may need multiple procedures during the same operation, depending on the case.
A retina specialist (ophthalmologist who specializes in retinal care) will base their decision on factors like age, the severity of detachment and which part of the retina is detached.
SEE RELATED: What is retinal detachment?
The three types of detached retina surgery are:
Scleral buckle
Scleral buckling surgery is a well-established type of treatment for retinal detachment. During the procedure, a silicone or plastic band is attached to the outside of the back portion of the sclera (the “white” of the eye).
The band gently “buckles” the eyeball inward, which reduces the amount of tension pulling on the retina. When the retina is no longer being pulled from the back of the eye, it slowly heals itself by reattaching to the tissue in the back of the eye.
The band will stay in place permanently after the procedure. It is placed toward the back of the eye, so you won’t be able to see it after surgery.
Scleral buckle surgery is usually performed under general anesthesia, which means you won’t be awake during the operation. Patients can usually go home on the same day of surgery, but won’t be able to drive themselves.
SEE RELATED: Types of retinal detachment
Pneumatic retinopexy
During a pneumatic retinopexy, a surgeon will inject a small gas bubble into your eye. Your eye will be positioned so the bubble will rest on the detached retina and hold it in place, allowing it to slowly reattach to the back of the eye.
In addition to an air bubble injection, the surgeon may use a laser (laser photocoagulation) or freezing (cryopexy) procedure to fix any retinal tears or holes.
After a pneumatic retinopexy, the patient will need to keep the bubble in place by maintaining the same head posture for several days.
Eventually the gas bubble will go away on its own. Activities like air travel, heavy lifting, vigorous exercise and scuba diving should be avoided until it disappears.
A pneumatic retinopexy is often done in the ophthalmologist’s office using local anesthesia around the affected eye.
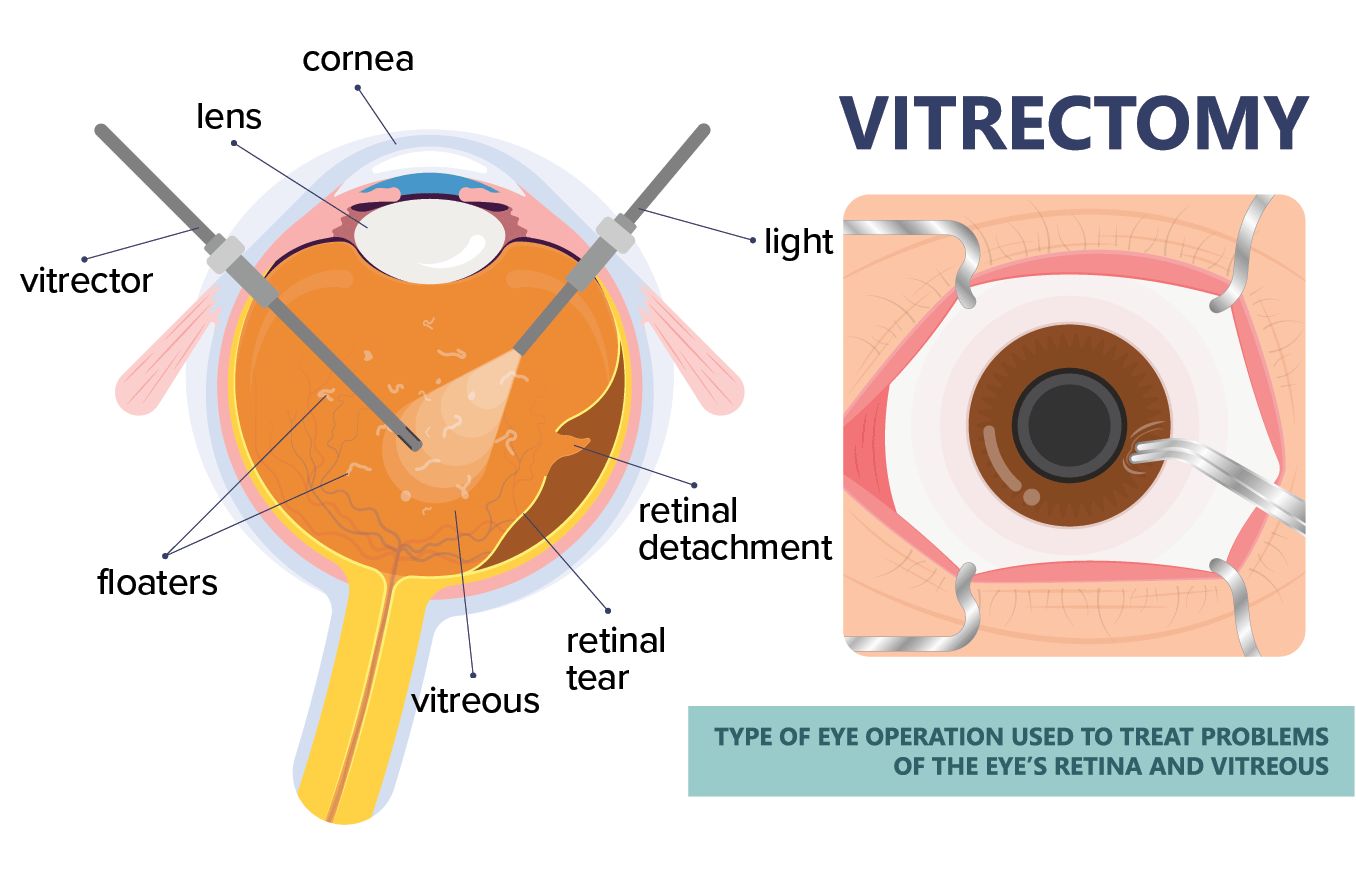
Vitrectomy
A vitrectomy involves removing some of the gel-like fluid called vitreous humor from inside the eye. The natural vitreous fluid is then replaced with a clear silicone oil, pushing the detached part of the retina back into place and allowing it to heal.
This can also be called pars plana vitrectomy, or just PPV.
Similar to a pneumatic retinopexy, a gas bubble can also be injected during a vitrectomy. In this case, the vitreous fluid will not be replaced by silicone oil. Instead, the body will produce its own fluid to replace the bubble as it dissolves.
A surgeon can choose to use either local or general anesthesia during a vitrectomy.
SEE RELATED: Retinal tear surgery
Recovery
The recovery process will depend on the patient’s condition and type of procedure(s) performed. Some level of discomfort can be expected after retinal detachment surgery, but it is usually easily managed with medication.
Postoperative patients will need to schedule routine eye exams afterward to monitor the health of the retina and treat any potential blurred vision after retinal detachment surgery.
Eyeglasses with impact-resistant polycarbonate lenses should be worn after surgery to prevent any future injuries to the retina. Life after retinal detachment surgery won’t require these lenses to be worn all the time, only during times when eye injuries are most likely to occur. Outdoor activities and contact sports are two common examples.
SEE RELATED: Retinal detachment surgery recovery
What is the success rate of retinal detachment treatment?
Surgery for a detached retina isn’t always successful, but success rates have improved over the years. A study by the Department of Ophthalmology and Visual Sciences, University of Louisville looked at more than 1,200 surgery patients and reached the following conclusions:
Patients who underwent the scleral buckle procedure had an 86% initial success rate.
Patients who underwent pneumatic retinopexy had a 68% initial success rate.
Patients who underwent the vitrectomy procedure had a 90% initial success rate.
Patients who required a combination of scleral buckling and vitrectomy had a 94% success rate.
Along with other factors, success rates will vary based on the location, cause and severity of a patient’s detached retina.
Retinal detachment is a medical emergency
If you think you’re suffering from a detached retina, schedule an appointment with an eye doctor as soon as possible. Retinal detachment can lead to blindness if left untreated.
While a detached retina can sometimes go days without damaging vision, early symptoms are often unnoticed. If you experience a sudden onset of eye floaters or flashes — especially if you also notice sudden blurry vision or loss of peripheral vision in one eye — contact an eye doctor immediately.
READ MORE: Detached retina symptoms
Page published on Tuesday, October 27, 2020






