What is 6th nerve palsy?
Sixth nerve palsy, also known as abducens nerve palsy, is a condition in which the sixth cranial nerve becomes paralyzed. This paralysis affects the lateral rectus muscle, which controls certain eye movements. It may affect one or both eyes, depending on the cause.
The condition is the most common ocular motor paralysis in adults. It’s second-most common in children, with fourth cranial nerve palsy being the most common.
Sixth nerve palsy symptoms often improve or resolve completely within a few months and may not require treatment. However, if your doctor doesn’t note any improvement over time, treatment or surgery may be needed.
Cranial nerve 6 function
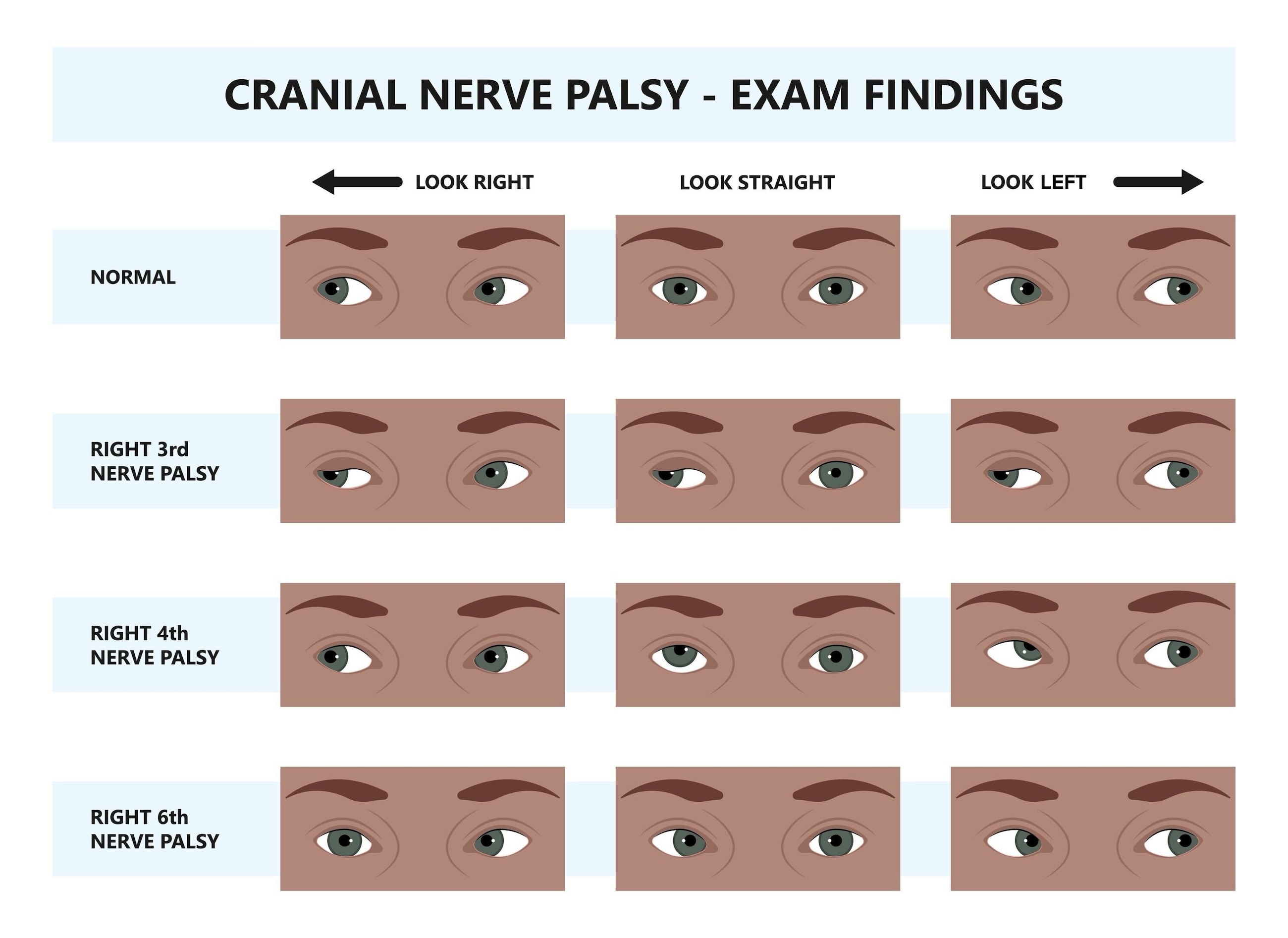
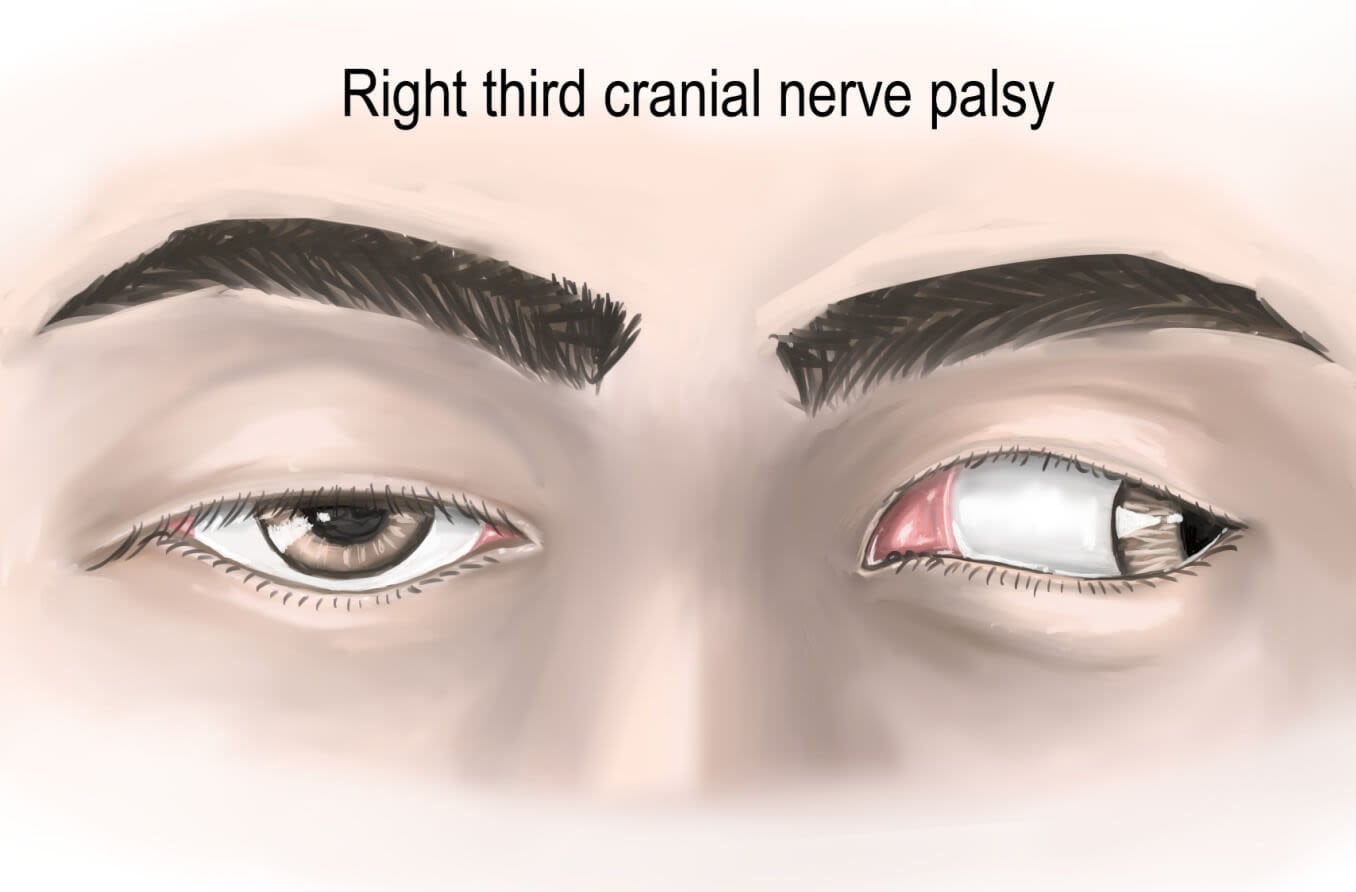
Cranial nerve 6 (the abducens nerve) is one of three nerves responsible for the extraocular movement of the eye. The other two nerves that aid in this function are cranial nerves three (oculomotor nerve) and four (trochlear nerve).
The abducens nerve specifically controls the lateral rectus muscle of the eye. This muscle allows you to move the eye outward, away from the nose. So, when you look to the left without moving your head, the lateral rectus muscle in your left eye controls that movement. Similarly, if you look to the right without moving your head, the lateral rectus muscle of your right eye is working.
When cranial nerve six palsy occurs, it eliminates or weakens the signal from the nerve to the muscle. This results in an inability to turn the affected eye(s) outward.
SEE RELATED: Crossed eyes (esotropia)
What causes cranial nerve palsy?
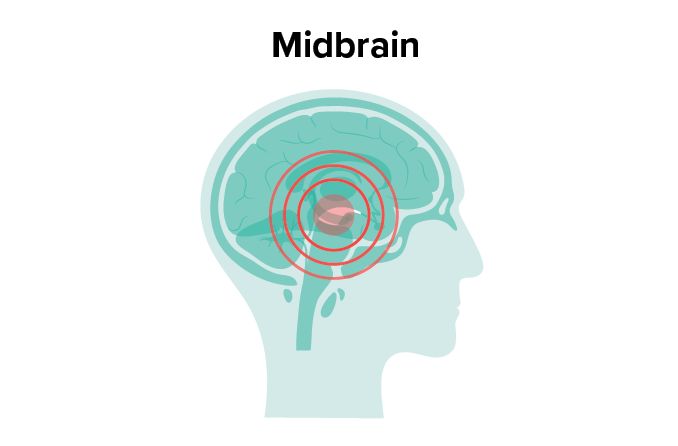
The 6th cranial nerve has the longest intracranial path of any cranial nerve. It begins in the brainstem and ends at the lateral rectus muscle, in the eye sockets. If a problem occurs at any point along the nerve’s journey, sixth cranial nerve palsy can result.
Some of the most common causes of cranial nerve palsy include:
- Inflammation of the abducens nerve
- Infection from a virus, fungus or bacteria
- Stroke
- Skull injury, especially if a fracture occurs
- Brain tumor or lesion
- Elevated or low pressure inside the brain, called intracranial pressure
- Deterioration of the nerve’s protective coating, often caused by multiple sclerosis
- Metabolic diseases, such as diabetes or Wernicke disease
- Meningitis
- Cavernous sinus thrombosis
- Pituitary tumor
Usually, these causes will create other symptoms in conjunction with 6th nerve palsy. If it occurs in isolation, meaning there are no other symptoms present, it may be caused by one of the following:
- Injury
- Virus
- Diabetes
- Hypertension (high blood pressure)
- Congenital cause
Sixth cranial nerve palsy may occur at birth — a condition known as congenital sixth nerve palsy. Congenital sixth nerve palsy is usually caused by trauma or injury that occurs during birth.
Trauma is the most common cause of 6th nerve palsy in children, whereas stroke is the most common cause in older adults.
It’s also possible for doctors to never determine a cause of sixth nerve palsy. In fact, up to 30% of sixth nerve palsy cases have a cause that is unknown.
SEE RELATED: Third Nerve Palsy
What are symptoms of sixth nerve palsy?
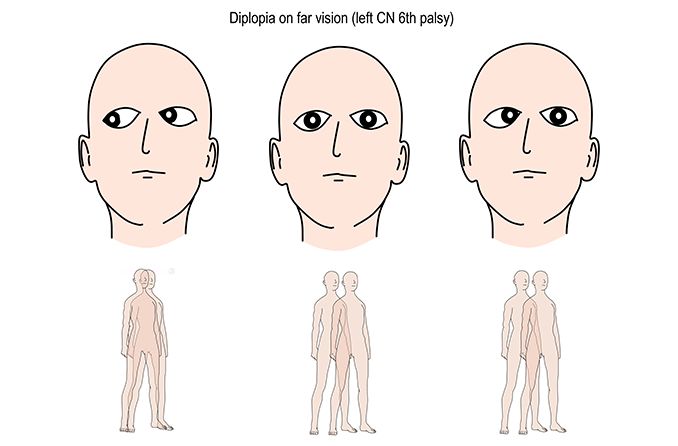
When isolated, sixth nerve palsy has only a few symptoms that affect the eyes and vision. The most common symptom is diplopia (double vision).
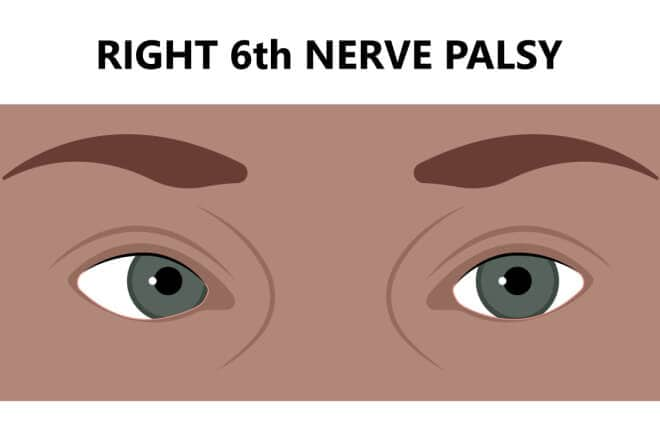
The type of diplopia experienced in 6th nerve palsy is horizontal diplopia. This type of diplopia creates a side-by-side effect of the two images. For example, if someone with horizontal diplopia was focusing on a bench, the faint “double” of the bench would be to the right or left of the actual object.
Diplopia is usually less severe when focusing up close, and gets worse when focusing at a distance.
Another symptom of isolated sixth nerve palsy is a misalignment of the eyes, known as strabismus. Sixth nerve palsy affects the muscle that allows the eyes to focus away from the midline. So, the affected eye may drift inward or stay focused ahead when it should be directed outward.
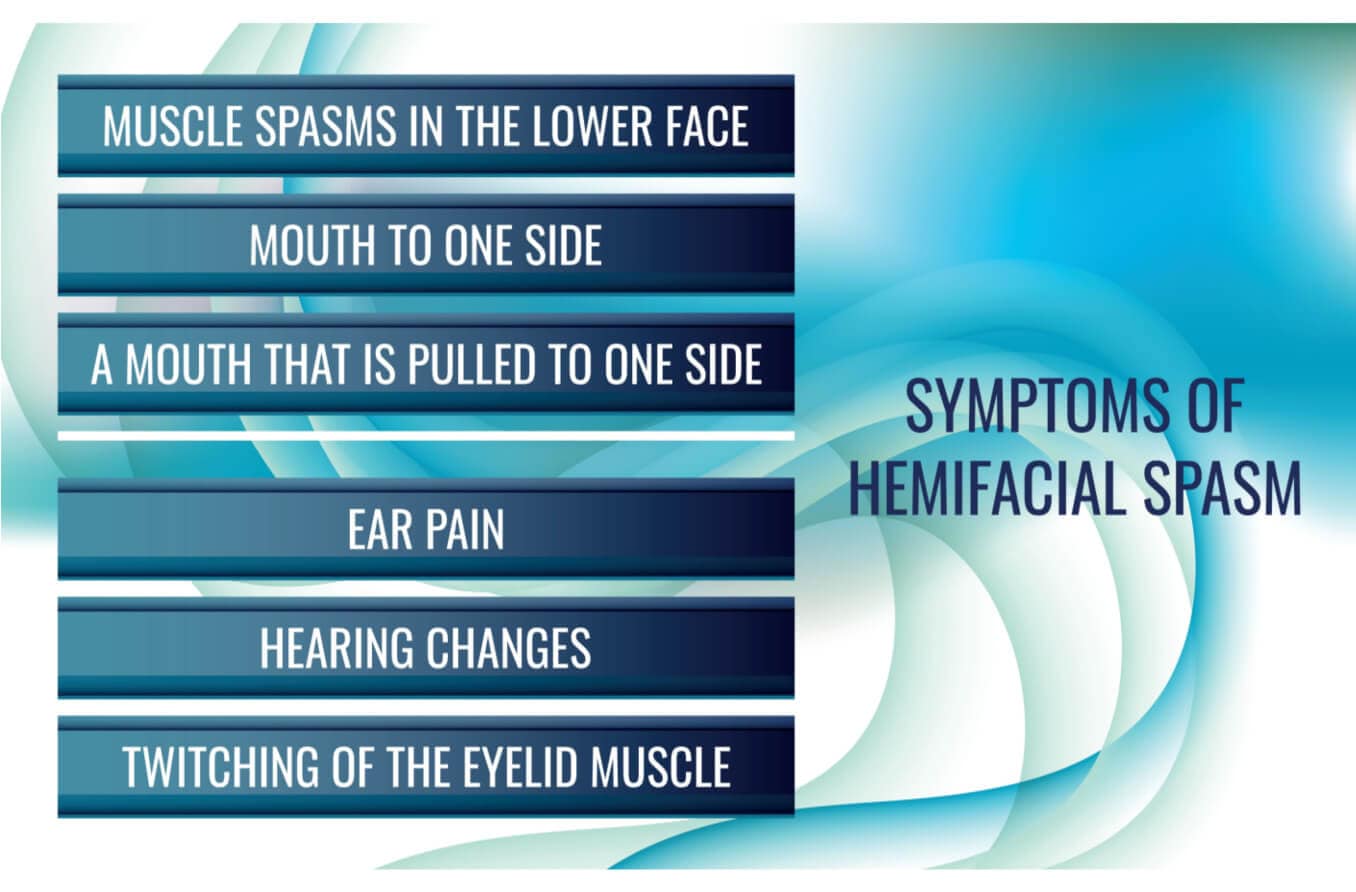
If other symptoms accompany sixth 6th nerve palsy, they usually consist of:
- Vision loss
- Facial weakness
- Loss or decrease in facial sensation
- Fever
- Pulsing or ringing in one or both ears (tinnitus)
- Headache
- Droopy eyelid (ptosis)
- Nausea and vomiting
- Hearing loss
SEE RELATED: Oscillopsia (Shaky Vision)
Risk factors for cranial nerve palsy
While it’s possible for cranial nerve palsy to occur spontaneously, there are certain conditions that can raise a person’s risk of experiencing sixth nerve palsy. These risk factors include:
- Poorly controlled diabetes
- Microvascular dysfunction (heart disease)
- Inflammatory diseases, such as multiple sclerosis, meningitis, encephalitis, cavernous sinus thrombosis, etc.
- High blood pressure
- High cholesterol
- Arteriosclerosis (plaque build-up in the arteries)
- Aneurysm
- Birth trauma
- Recent history of viral infection
To lower your risk of sixth nerve palsy, it’s important to monitor your blood pressure, cholesterol, and underlying conditions. Having regular physical exams and practicing a healthy lifestyle can reduce your chances of developing serious conditions later in life.
SEE RELATED: What your eye doctor can tell about your heart health
Treatment and prognosis
Treatment for sixth cranial nerve palsy depends on the cause. In most cases, the muscle weakness should improve within six months. Isolated 6th nerve palsy is more likely to resolve completely than cases with additional symptoms.
Possible treatments for sixth cranial nerve palsy include:
- Corticosteroids for cases caused by inflammation
- Antibiotics for cases caused by bacterial infection
- Surgery, chemotherapy and/or radiation for cases caused by brain tumors or lesions
- Surgery or lumbar puncture for cases caused by increased intracranial pressure
The goal of congenital cranial nerve palsy is to prevent amblyopia, which can negatively affect a child’s vision. So, unlike adults, children will also receive patching treatment. Patching consists of covering one eye at a time with an eye patch. The eye should stay covered for a set amount of time, as advised by your eye doctor. Once that time is up, you switch the patch to the other eye.
Patching can help with double vision and decreases the possibility of ipsilateral medial rectus contracture. This is the permanent tightening of the medial rectus muscle — the muscle on the opposite side of the eye from the lateral rectus muscle.
Other management and treatment options for sixth cranial nerve palsy include:
- Wearing prism glasses that assist with aligning the eyes
- Injecting botulinum toxin (botox) in the opposite muscle of the affected eye to help eye alignment
If the above-mentioned treatments don’t improve your symptoms after six months, you may need strabismus surgery. This procedure consists of adjusting muscles within the eye to help strengthen and align it properly. A full recovery can take up to six weeks, and results may vary.