Photodynamic therapy: How it works and the benefits of PDT

What is photodynamic therapy (PDT)?
Photodynamic therapy (PDT) is a procedure that uses light and special medications to treat harmful cells. The medications used in PDT are light-sensitive, meaning they are only activated once they have been exposed to light.
The light is typically administered by a laser or light-emitting diode (LED). This allows for a targeted effect on the impacted area.
PDT can be used to treat a number of conditions. Some of these include cancer, skin conditions, age-related macular degeneration and certain infections.
How does photodynamic therapy work?
Photodynamic therapy involves certain drugs known as photosensitizing agents. This means that they do not work until light hits them. The physician will either place the agent directly onto the skin or inject it into the bloodstream. The location depends on the condition being treated.
There is a waiting period after the medication is applied, called the drug-to-light interval. This period allows the cells to absorb the drug. Depending on the drug itself, the wait can last between a few hours and a couple of days. Once the drug has been absorbed, the physician will apply light.
The type of light the physician uses will depend on the location and type of abnormal cells they are targeting. When light hits the medication, it causes the drug to form an oxygen molecule (reactive oxygen species) that then kills the surrounding cells.
It may also destroy some of the blood vessels that support the abnormal cells’ growth. In turn, this may alert the body’s immune system to attack the cells as well.
What is photodynamic therapy used for?
Photodynamic therapy is useful for treating areas in the body that light can reach. These include the skin, eyes, mouth, esophagus and lungs.
Some conditions that PDT can be used to treat include:
Skin conditions, such as psoriasis, actinic keratosis and vitiligo
Various forms of cancer
Urinary tract infections
Acute sinusitis
Gastritis
Gum disease
Age-related macular degeneration
One condition that photodynamic therapy can help with is age-related macular degeneration (AMD). AMD is a disease found in the macula — an area of tissue at the center of the retina.
The retina is a layer of cells lining the back of the eye. It is responsible for turning light into nerve signals. These signals are then sent through the optic nerve to the brain, where they are interpreted into the images we see. The macula is responsible for central vision, or what is right in front of the eye.
AMD occurs with age. As it damages the macula, it blurs central vision. This can make things like reading, driving, cooking and seeing faces more difficult. It is the most common cause of vision loss in older adults.
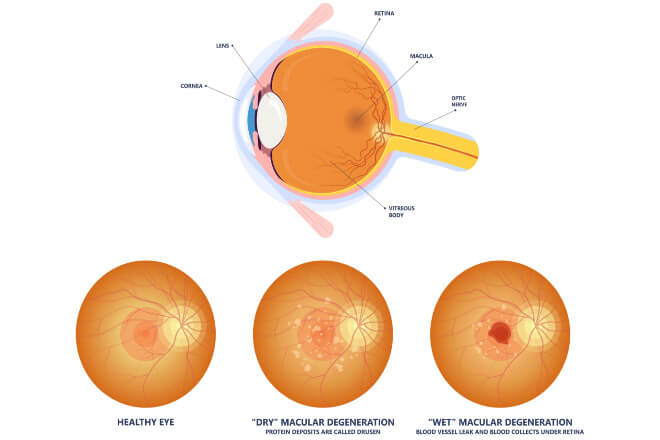
Healthy eye as compared to an eye with dry macular degeneration and wet macular degeneration.
AMD comes in two forms: dry and wet. The dry version is more common, occurring as the macula thins with age. The wet version develops with the growth of abnormal blood vessels in the back of the eye. These blood vessels damage the macula.
Photodynamic therapy can be used to help treat wet AMD. It can slow down the loss of central vision by targeting these abnormal blood vessels. PDT cannot repair existing vision loss, but it can help slow further damage. The photosensitizing agent does this by clotting the blood in the abnormal vessels, which seals them off.
Due to the development of medications that can impede the growth of abnormal blood vessels, PDT is not used as often for treating AMD. However, it may be combined with these medications for more effective treatment. Consult with your eye doctor about the appropriate AMD treatment for you.
Other eye conditions treated with PDT
There are several other eye conditions that can be treated with photodynamic therapy, including:
Central serous chorioretinopathy – A condition brought on by fluid buildup in the macula. This buildup can lead to impaired central vision and visual distortion (metamorphopsia).
Polypoidal choroidal vasculopathy – A maculopathy that causes reddish lesions on the choroid.
Peripapillary choroidal neovascularization – A condition in which blood vessels form too close to the optic nerve head.
Multifocal choroiditis and punctate inner choroidopathy – Inflammatory conditions that cause yellowish lesions. These lesions typically form on the choroid and retina.
Ocular histoplasmosis – A fungal infection that can cause blood vessels to grow where they shouldn’t. It can impact a variety of organs. If it affects the eyes, it can lead to vision loss, depending on where the new vessels develop.
Choroidal hemangiomas – Benign (non-cancerous) tumors that can develop in the retina. These typically appear as reddish domes on the back of the retina.
Retinal capillary hemangioblastomas – Benign tumors that develop on the middle or edge of the retina.
Choroidal nevus – A benign tumor that develops near the center of the retina. This is the most common type of tumor found in the eye.
Choroidal melanoma – A cancerous (malignant) tumor that can develop in the choroid.
Idiopathic Juxtafoveal Telangiectasia (Macular Telangiectasia) – a rare condition due to abnormal blood vessels surrounding the fovea.
What are the benefits and side effects of photodynamic therapy?
Photodynamic therapy has several benefits. When done properly, there are no known long-term issues associated with PDT. The procedure is short and can be repeated if needed. It is less invasive than surgery, and typically causes minimal scarring.
PDT also allows for more precise targeting of treatment and may cost less than other, more intensive procedures.
However, every medical procedure comes with some risk. The use of photosensitizing agents can make patients more sensitive to light. For some, the eyes and skin may remain extra sensitive to light for up to three months post-procedure. This is because the light-sensitive medications affect both normal and abnormal cells.
For those receiving PDT for the eyes, side effects may include:
Pain at the injection point
Temporarily blurred vision
For those receiving PDT on the skin, side effects may include:
Swelling around the treated area
Discoloration
Scales or blisters around the treated area
Itching or burning
Skin infection
For those receiving PDT on the esophagus, side effects may include:
Hiccups
Difficulty swallowing
Nausea
Vomiting
Dehydration
Fever
For those receiving PDT on the lungs, side effects may include:
Shortness of breath
Infections, such as pneumonia or bronchitis
Coughing up blood
Fever
Depending on the area being treated, it can take between two and six weeks to fully heal from PDT.
What is the outlook after photodynamic therapy?
As a treatment for certain cancers, PDT has shown a similar success rate as chemotherapy or radiation. For those receiving it as treatment for other conditions, including AMD, it is only a semi-permanent solution.
After the PDT procedure, most individuals can return to their normal activities immediately. However, temporary lifestyle changes may be necessary if the patient experiences strong light-sensitivity.
Getting photodynamic therapy. American Cancer Society. November 2021.
Photodynamic therapy. Mayo Clinic. March 2022.
Photodynamic therapy (PDT). Cleveland Clinic. April 2022.
Photodynamic therapy (PDT). National Health Service. November 2019.
Photodynamic Therapy for Age-Related Macular Degeneration. Johns Hopkins Medicine. Accessed February 2023.
Macula. Cleveland Clinic. May 2022.
Age-Related Macular Degeneration (AMD). National Eye Institute. June 2021.
Page published on Tuesday, March 7, 2023
Page updated on Tuesday, March 14, 2023
Medically reviewed on Wednesday, February 1, 2023






