Clogged tear ducts in a baby: Causes, symptoms and treatment
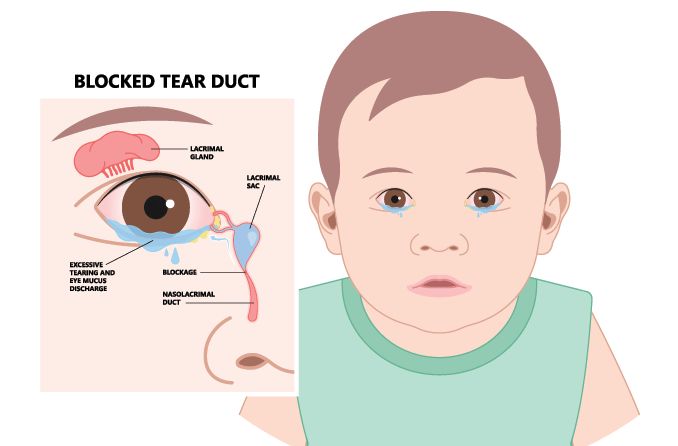
A blocked tear duct in a baby is a common condition that affects how well the infant can drain their tears. Babies are most susceptible to tear duct obstructions because their tear duct system is not fully developed.
Clogged tear ducts in newborns will normally resolve on their own within their first year of life. In the meantime, there are home and clinical treatment options that may help open blockages and relieve the excessive tearing.
Causes
Blocked tear ducts can be caused by several factors when seen in adults, including injury or age-related narrowing of the tear ducts. Cases of newborn blocked tear ducts are typically caused by:
The thin membrane at the end of the tear duct — known as the valve of Hasner — failing to open correctly. This is the most common cause of clogged tear ducts in newborns.
Craniofacial abnormalities that cause irregular nasal bone growth.
A tumor that may be putting pressure on the nasolacrimal (tear drainage) system.
Infection, such as conjunctivitis, may spread to the tear duct, causing a blockage.
Puncta (the eyes’ inner corner openings to the tear ducts) that are underdeveloped or closed, making it impossible for tears to drain.
Approximately 6% to 30% of babies are born with a blocked tear duct. In most cases, the tear ducts spontaneously open and drain normally within the first year of life.
Blocked tear ducts typically do not affect a baby’s vision, and there is no evidence that having blocked tear ducts as a newborn will cause future eye problems.
Symptoms
A clogged tear duct in a baby can lead to a case of bacterial conjunctivitis when the tear duct becomes infected. It’s important to understand the symptoms associated with a blocked tear duct so proper treatment can be administered.
Symptoms commonly observed in a baby with blocked tear ducts include:
Excessive tearing, which may collect in the inner corner of the eye (known as the lacrimal lake) or spill out onto the cheeks
White or yellowish eye discharge
Crusty eyes or eyelashes, usually present after sleeping
Swelling and/or tenderness near the inner corner of the eye
Redness around the eye, but not the eye itself
When a blocked tear duct goes untreated, it can lead to dacryocystitis, an infection of the tear duct. Symptoms of infection can include:
Pain, swelling and redness of the inner corner of the eye. Severe cases may also present bruising
Fever
Eye redness
Blood-tinged tears
If you notice these symptoms in your baby, their blocked tear duct may have become infected. It’s recommended that you take your baby to a pediatric eye doctor, who can assess their symptoms and determine proper treatment.
Diagnosis
A pediatric eye doctor will be able to determine whether your baby has a blocked tear duct based on the symptoms they exhibit.
Though an eye exam is usually enough to form a diagnosis, they may choose to conduct certain tests to confirm it, including a modified fluorescein dye disappearance test.
In the modified fluorescein dye disappearance test, a fluorescein dye is put into your baby’s eyes. After five minutes, the eye doctor will use a blue light and shine it into the child’s eyes and nasal passages.
If the dye is:
Still visible in the eye, a blockage is likely somewhere within the tear duct system.
Untraceable in the eye, it means the tear duct is draining tears normally.
Detectable in the nasal passages, this also supports that the tear duct is open and draining normally.
Treatment
A baby’s blocked tear duct often doesn’t require treatment. In many cases, the membrane blocking the duct will open on its own and the drainage system will develop completely by nine to 12 months of age.
In the meantime, here are some home treatment options that may help your baby feel more comfortable:
Gentle cleaning of the eyes
Dampen a clean washcloth or cotton ball with warm water and gently clean your baby’s eyes, starting at the inner corner and moving out toward the outer corner. If you are having to clean discharge from your baby’s eyes more than two or three times per day, your pediatrician may prescribe antibiotic eye drops.
Warm compress
A warm compress applied to the affected eye will help to soften the tissue in the area and encourage spontaneous opening of the duct. Using a warm compress prior to nasolacrimal massage improves the effectiveness of the massage treatment. Allowing heat to remain on the affected area for five to 10 minutes is ideal.
Nasolacrimal massage
If recommended by your doctor, use clean hands to gently massage the space between the inner corner of your child’s affected eye and their nose. Press in and down for a few seconds, then release.
This technique should be repeated 10 times per affected eye, twice per day (preferably morning and night). The goal of nasolacrimal massage is to put pressure on the lacrimal sac and have it coax the valve of Hasner open.
Surgical intervention
In severe cases, a pediatric ophthalmologist may consider a more invasive medical procedure that must be performed under anesthesia. However, these are typically performed on older patients:
Probing and irrigation
This medical procedure is used for babies whose tear ducts will not open up on their own. This is a last resort treatment for tear ducts that have not opened or patients with chronic infections.
The punctal openings are dilated using an instrument, then a tiny probe is snaked through the tear duct drainage system and removed from the nasal opening. After that, a saline solution is used to flush the drainage system of any leftover blockages. Patients are under anesthesia during this procedure done by a pediatric ophthalmologist in an operating room.
Widening drainage passages
Under general anesthesia, a pediatric ophthalmologist will insert a narrow catheter into the nasolacrimal duct. Once in place, the doctor will inflate the catheter like a balloon to widen the passages, then deflate it before removing. This procedure is used on individuals whose passageways are narrowed due to inflammation or scarring. This is not a typical treatment procedure for young children.
Stenting
This procedure consists of having thin tubing threaded through the entire drainage system, from the puncta to the nasal opening. The tubing is left in the nasolacrimal system for three to four months before it’s removed. Patients are under general anesthesia during this procedure. This is not a typical treatment procedure for young children.
When to see a doctor
If you have any concerns about your baby’s eyes or vision, don’t hesitate to take them to their pediatrician or a pediatric eye doctor. Even if the problem seems minor, like blocked tear ducts, they can assess your child’s condition and recommend the best course of action.
READ MORE: Baby’s first eye exam: What to expect
What causes a blocked tear duct in infants?. Medical News Today. July 2018.
Blocked tear ducts. C.S. Mott Children’s Hospital. May 2020.
Blocked tear duct in children. Verywell Health. November 2019.
What is a blocked tear duct?. American Academy of Ophthalmology. March 2015.
Page published on Thursday, July 29, 2021
Medically reviewed on Thursday, July 29, 2021






