Maculopathy: Causes, symptoms, types and treatment

On this page:
What is maculopathy?
What are the symptoms of maculopathy?
What causes maculopathy?
What are the different types of maculopathy?
How is maculopathy treated?
How can I decrease my risk of maculopathy?
On this page:
What is maculopathy?
What are the symptoms of maculopathy?
What causes maculopathy?
What are the different types of maculopathy?
How is maculopathy treated?
How can I decrease my risk of maculopathy?
What are the symptoms of maculopathy?
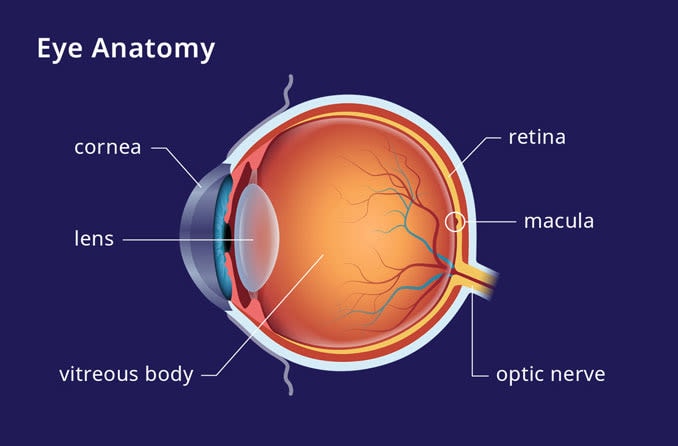
The macula is responsible for the fine detail provided by your central vision. It is the location of a high concentration of photoreceptor cells called rods and cones. These cells convert light into electrical signals that are sent to the brain to be processed as images. Damage to these cells can result in severe central vision loss.
Fine-detail vision is essential for many daily tasks such as cooking, reading, watching television and reading signs while driving. Because the macula is responsible for central vision, peripheral vision is usually not affected in maculopathy.
Symptoms of maculopathy include:
- Decreased visual acuity
- Distorted vision
- Poor color vision
- Blind spot in central vision
- Light sensitivity
- Difficulty seeing in low light levels
What causes maculopathy?
The macula can be injured due to a number of eye diseases and conditions. The most common causes of damage to the macula include age-related macular degeneration (AMD) and diabetic retinopathy (DR).
Age-related macular degeneration
Age-related macular degeneration is damage to the macula caused by aging. It can occur with proliferation and leaking of abnormal blood vessels (wet AMD). It can also occur without leaking blood vessels (dry AMD). Most cases of AMD (about 80%) are the dry form. This is when the macula becomes thin and clusters of protein, called drusen, accumulate. This leads to a gradual loss of central vision.
Diabetic retinopathy
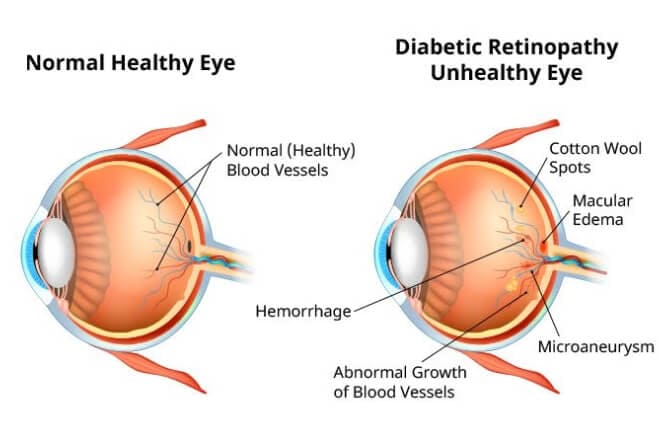
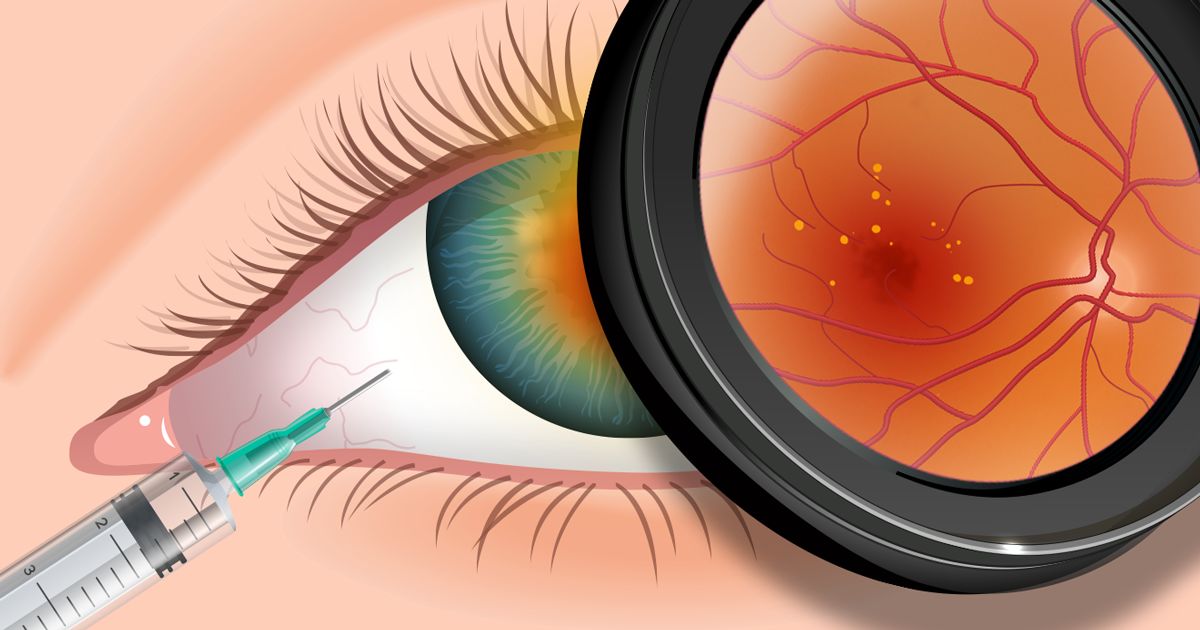
Click on image to enlarge.
Diabetes results in excess sugar circulating in the blood vessels of the body. As a result, the body’s blood vessels begin to weaken and leak. Diabetic retinopathy can cause blood vessel leakage in the retina.
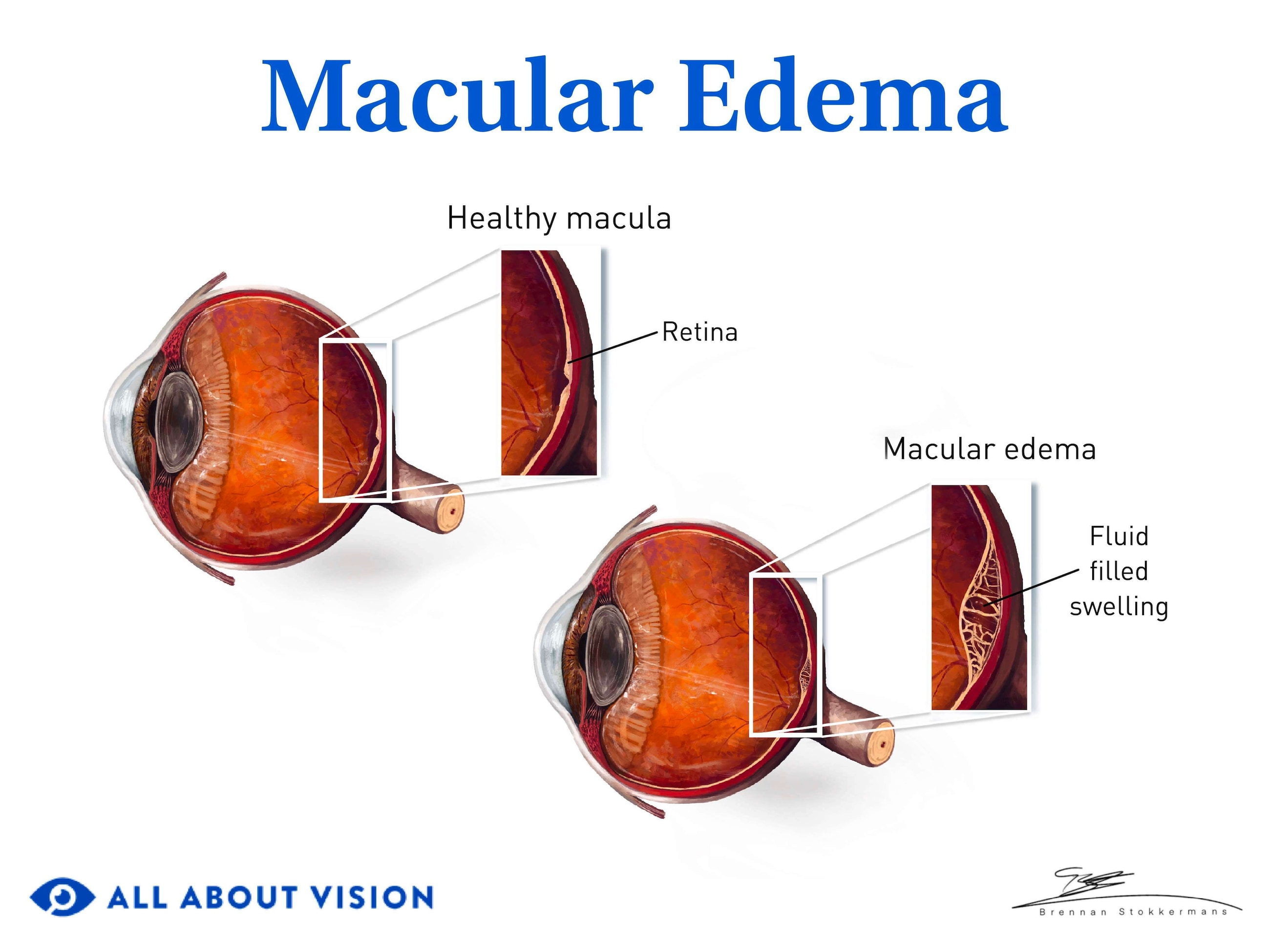
Macular edema
Leaking blood vessels in the retina are a common cause of damage to the macula. They are often due to diseases such as AMD and diabetic retinopathy, and can lead to a condition called macular edema. Macular edema occurs when the macula swells and becomes thick due to fluid build-up. This leads to distorted and blurry central vision. It can also decrease color vision.
Other causes of macular edema are:
- Complications due to eye surgery
- Retinal blood vessel blockage
- Inflammatory diseases leading to retina damage
READ MORE: Diabetic eye exams: What to expect
What are the different types of maculopathy?
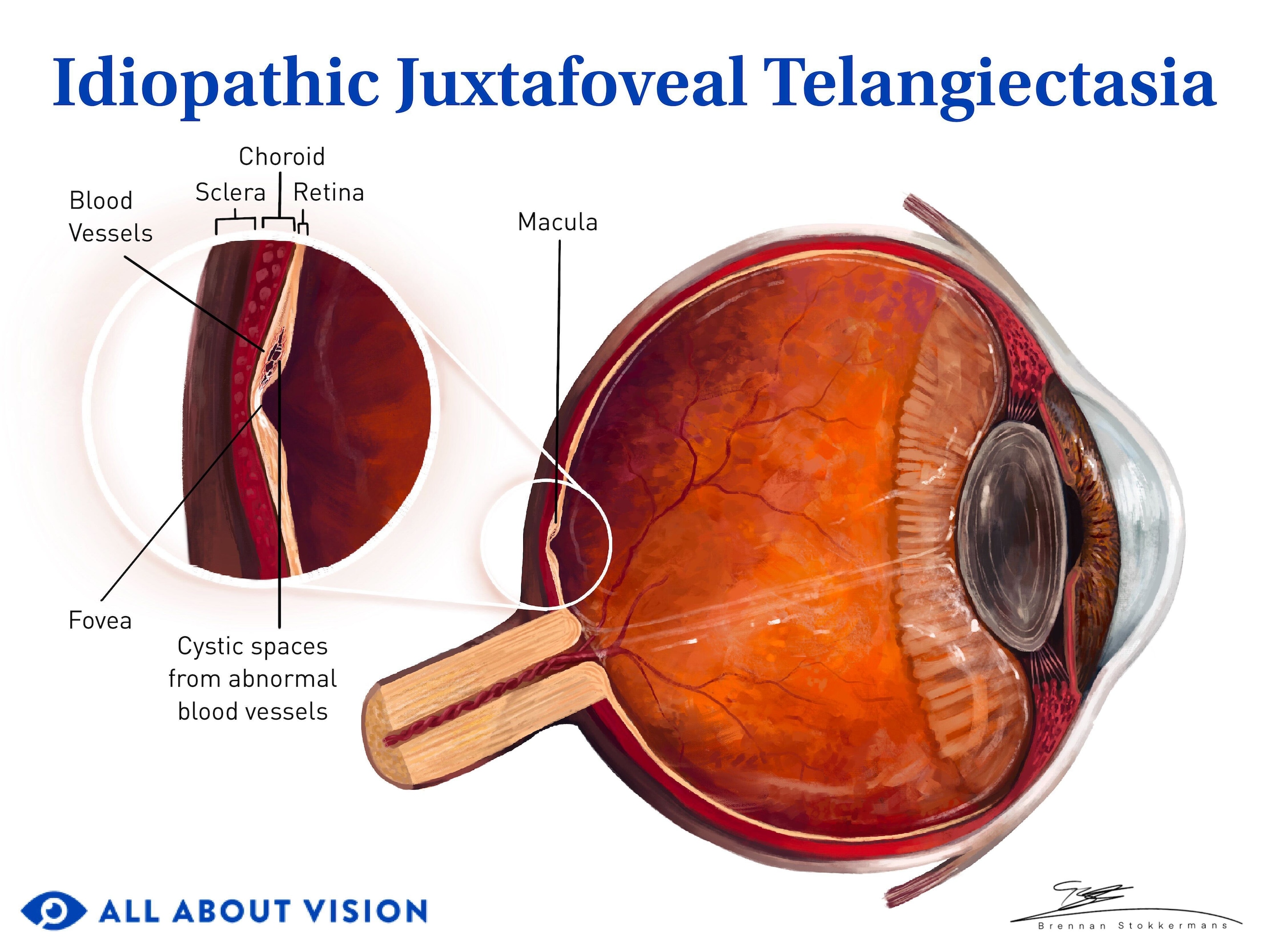
While AMD and diabetic retinopathy are common causes of maculopathy, there are specific types of maculopathy that also cause damage to the macula:
Myopic maculopathy
Myopic maculopathy is also known as myopic macular degeneration. It is damage to the macula from progressive, abnormal elongation of the eyeball which has resulted in degenerative changes in the back of the eye. It is seen in pathological myopia, or degenerative myopia, which is a leading cause of vision impairment worldwide.
The lengthening causes the retina and back of the eyeball to stretch. This results in thinning and degenerative changes to the retina, choroid and sclera. Two important factors are associated with pathological myopia:
- Elongation of the eyeball – An increase in the eyeball’s axial length (distance from the front of the eye to the back of the eye).
- Presence of posterior staphyloma – An outpouching of the wall of the back of the eyeball. It is one of the major factors that leads to myopic maculopathy.
These changes can lead to permanent visual impairment and blindness. In addition to central vision loss, a 2021 study published in British Journal of Ophthalmology suggests that adults with high myopia and myopic macular degeneration may experience visual field loss.
Bull's eye maculopathy
Bull’s eye maculopathy is a description used by doctors to describe the appearance of the macula when it’s surrounded by circular bands of pale, damaged areas. This bull’s eye appearance of the macula may be due to many different conditions, including:
- Medication-related maculopathy – Long-term use of medication that treats rheumatoid arthritis or lupus such as chloroquine or hydroxychloroquine (Plaquenil).
- Juvenile macular degeneration (Stargardt’s disease) – A rare, genetic condition that causes gradual vision loss in both eyes, typically starting in childhood.
- Cone dystrophies – Rare eye diseases that cause damage to the retina’s cone photoreceptor cells. Symptoms include decreased visual acuity, poor color vision and light sensitivity.
- Benign concentric annular macular dystrophy (BCAMD) – A rare dystrophy that can cause vision loss that ranges from mild to severe.
- Batten’s disease – A group of rare genetic conditions that result from a metabolic disorder. It results in vision loss, seizures, cognitive and movement issues, and a short life expectancy.
Pigmentary maculopathy
This maculopathy is due to the chronic use of the drug Elmiron (pentosan polysulfate sodium). This medication is used in the treatment of interstitial cystitis, a syndrome which results in inflammation and pain in the bladder.
Visual acuity may be affected by the subtle depositing of pigment in the macula. Patients describe difficulty reading and adapting to low light.
Cellophane maculopathy
Cellophane maculopathy causes distorted and blurry central vision. It is the result of abnormal growth of a cellophane-like tissue, or membrane, over the macula. This condition is referred to by several other names, including:
Macular pucker, also known as epiretinal membrane, is a thin, film-like tissue that can form over the macula and cause distorted, blurry vision. [Image credit: Macular pucker. Permission granted by © 2022 American Academy of Ophthalmology]
- Macular pucker
- Epiretinal membrane
- Surface-wrinkling retinopathy
Growth of this thin tissue over the macula can be a result of:
- Disease, such as diabetic retinopathy or uveitis
- Cataract surgery
- Injury
- Retinal detachment or retinal tear, which then leads to eye inflammation
- No identifiable cause
Since vision changes are usually mild and typically only affect one eye, treatment may not be needed. But if vision is severely affected, a surgery such as vitrectomy with membrane peel may be recommended. This procedure removes the vitreous gel of the eye and peels away the cellophane-like tissue over the macula. This outpatient surgery is usually quite successful and typically improves vision.
Solar maculopathy
Damage to the macula from looking at the sun (sun gazing) or viewing an eclipse can result in decreased visual acuity or a central blind spot. Although vision is usually only affected for 3 to 6 months, permanent vision loss can occur. Solar maculopathy is also known as:
- Solar retinopathy
- Solar retinitis
- Eclipse retinopathy
- Photic retinopathy
- Foveomacular retinitis
In solar maculopathy, the macula is injured by heat and chemical damage from prolonged exposure to sunlight. Doctors can use a procedure called optical coherence tomography (OCT) to diagnose the condition. OCT allows them to see the layers of the retina that may have been damaged by the sunlight.
Children and other young people have a higher risk of damage to the macula from sunlight because the eye’s lens hasn’t fully developed the ability to block UVB light (that protection grows with age). Certain medications such as tetracycline can also increase risk of injury to the macula from intense sunlight exposure. If vision has not improved within six months, the prognosis is poor that it will return to normal.
How is maculopathy treated?
The macula can be damaged due to a number of eye diseases and conditions. Due to this, the specific treatment plan will vary. In general, treatments focus on reducing neovascularization, the growth of new leaky blood vessels. This is done to prevent irreversible vision loss, which is a common complication of retinal neovascularization.
Anti-VEGF therapy
Anti-VEGF therapy has been found to be effective in treating maculopathy. This involves injecting the eye with medicine such as intravitreal bevacizumab (Avastin) and ranibizumab (Lucentis) that reduces the growth of abnormal blood vessels.
Photodynamic therapy
Another treatment that can be effective is photodynamic therapy . This is an in-office procedure that uses a laser and a medicine (Verteporfin) to seal off leaky, abnormal blood vessels.
Vitrectomy
Finally, if traction at the macula is noticed, a vitrectomy may be performed. This is a surgical procedure in which the vitreous (the gel-like substance that fills the middle of the eye) is removed and replaced with a saline fluid.
This surgery is performed to prevent vision-threatening complications that may result from the vitreous tugging at the macula.
SEE RELATED: Vitreomacular traction syndrome
How can I decrease my risk of maculopathy?
Underlying conditions that cause maculopathy, such as AMD and diabetic retinopathy, have certain risk factors like age, smoking and obesity. To decrease your risk of developing eye disease include, it is recommended that you:
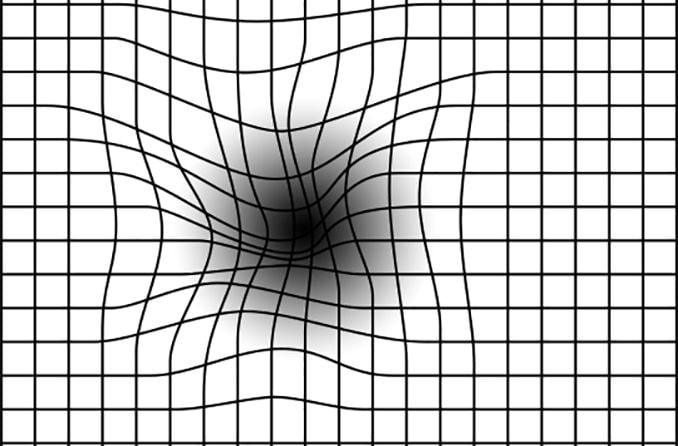
An Amsler grid consists of straight lines, with a reference dot in the center.
Don’t smoke – Smokers have two times the risk of developing AMD.
Eat a healthy, nutritious diet – Eat plenty of leafy green vegetables, fruits and low-fat foods.
Exercise – Get active for 30 to 60 minutes a day, for a total of at least 150 minutes (2.5 hours) each week.
Watch your weight – Obesity greatly increases the risk of developing eye and heart disease.
Wear sunglasses – Make sure that your sunglasses are labeled as having 99% to 100% UV protection .
According to some studies, people with certain types of macular disease, such as dry AMD, may benefit from nutritional supplements . Speak to your eye doctor for recommendations on taking eye vitamins for your particular condition. In addition, if you were given an Amsler grid to monitor your vision, check it on a daily basis.
And remember: Routine, comprehensive eye exams are the first step toward maintaining healthy eyes and clear vision.
On this page:
What is maculopathy?
What are the symptoms of maculopathy?
What causes maculopathy?
What are the different types of maculopathy?
How is maculopathy treated?
How can I decrease my risk of maculopathy?
On this page:
What is maculopathy?
What are the symptoms of maculopathy?
What causes maculopathy?
What are the different types of maculopathy?
How is maculopathy treated?
How can I decrease my risk of maculopathy?