What is pseudoexfoliation syndrome?
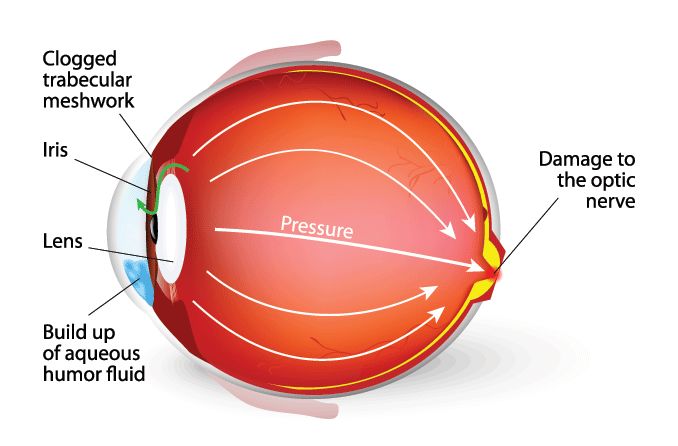
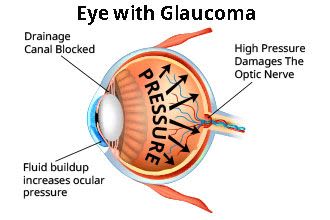
Pseudoexfoliation syndrome is when tiny clumps of protein fibers form in and around the body, including in the front of the eye. These clumps, that look like dandruff flakes, can clog the eye’s drainage area and raise eye pressure, eventually leading to glaucoma, cataracts and possible vision loss.
While they are only harmful in the eyes, the flakes can also build up in the lungs, skin, heart and kidneys. Pseudoexfoliation syndrome (also called PXF, PXE or PEF) involves these parts of the eye:
- Aqueous humor. The clear, watery fluid in the front of the eye that provides the eye with nourishment, removes waste, and maintains normal eye shape and pressure
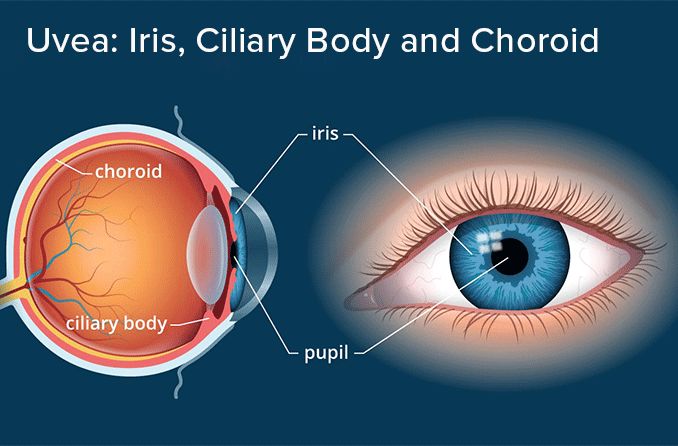
- Ciliary body. Holds the natural lens in place behind the pupil, enables accommodation of the eyes and produces aqueous fluid
- Cornea. The clear outer part at the front of the eye that focuses the light allowed in by the pupil
- Iris. The colored part of the eye that adjusts the size of the pupil to control how much light reaches the back of the eye
- Lens. The clear part of the eye behind the iris that allows the eye to focus on objects close up and far away
- Pupil. The opening at the center of the iris that lets light enter the eye
- Trabecular meshwork. Porous, spongy tissue within the drainage angle of the eye; fluid exits the eye here
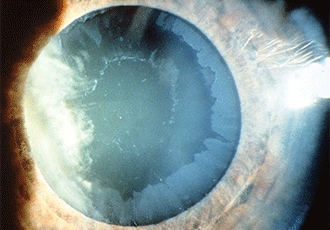
Pseudoexfoliation [Image credit: Permission granted by © 2022 American Academy of Ophthalmology]
Here’s how pseudoexfoliation occurs within the eye:
- As your pupil contracts and expands, the iris may brush over and against the lens.
- This brushing can rub very small flakes off of the lens.
- These flakes collect mostly in the front of the eye: on the lens, along the edges of the pupil, between the cornea and iris, and in the trabecular meshwork.