Understanding meibomian gland dysfunction
Meibomian gland dysfunction (MGD) is a very common eye problem. It is inflammation and clogging of the meibomian (my-BOH-me-an) glands in your eyelids. These glands produce the oil (meibum) in tear film that helps keep it from drying up. When tears evaporate too quickly, it leads to dry, irritated eyes.
MGD is a leading cause of evaporative dry eye disease (EDE). It can be easy to confuse MGD and EDE, but they are separate conditions. Other medical terms for meibomian gland dysfunction are meibomitis and meibomianitis.
Signs and symptoms of meibomian gland dysfunction
In addition to dry eyes, signs and symptoms of meibomian gland dysfunction (MGD) can include:
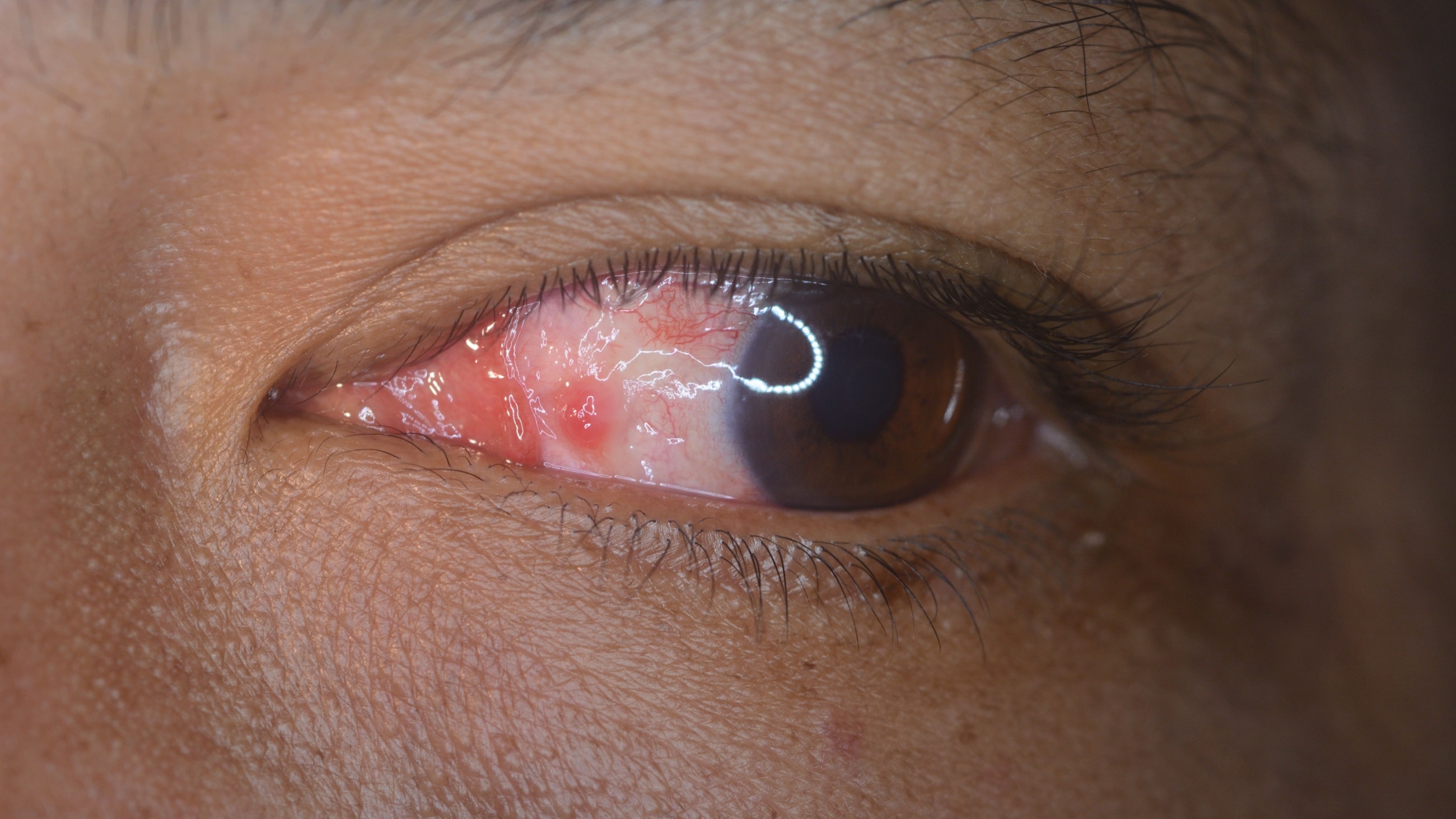
- Red eyes
- Itchy eyes
- Burning eyes
- Watery eyes
- Sensitivity to light
- Foreign body sensation (feeling like something is in your eye)
- Intermittent blurry vision
Meibomian gland dysfunction often occurs with blepharitis. This condition causes inflamed eyelids and a crusty discharge at the base of the eyelashes.
Styes also occur frequently with MGD, causing a sensitive red bump at the eyelid margin. And sometimes, meibomian gland dysfunction can cause a painless bump inside the eyelid. This is called a meibomian cyst or chalazion.
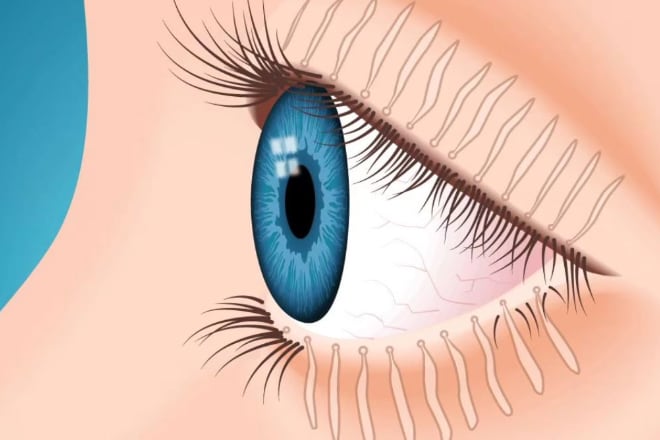
Other conditions that can occur with MGD include trichiasis and acquired distichiasis. Both affect the eyelashes. Trichiasis is a condition in which the eyelashes grow inward and irritate the eyes. In acquired distichiasis, an extra row of eyelashes grows from within the meibomian glands.
Other conditions that can occur with MGD include
MGD risk factors
Aging increases your risk of dry eyes and meibomian gland dysfunction. In fact, about 70% of people over age 60 have MGD. Researchers think this may be due to a natural decrease in the activity of stem cells that regulate these glands.
Your ethnic background may also play a role. Many studies have shown that up to 69% of Asian populations have MGD, compared to only 20% to 30% of white populations. However, these results can vary a lot based on the criteria used in the research.
Wearing contacts can also aggravate meibomian gland dysfunction. Several studies have linked contact lens wear with MGD but without a clear cause. For example, more frequent eye rubbing or cosmetics buildup on the lenses could be factors.
Wearing eye makeup is another contributing cause of MGD. Eyeliner and other makeup can clog the openings of meibomian glands. This is especially true if you don't thoroughly clean your eyelids of eye makeup before sleep. But remember to be gentle. Aggressive, frequent eye makeup removal may also harm meibomian glands.
Other possible risk factors include:
- Demodex mites (eyelid or eyelash mites)
- Androgen (a hormone) deficiency
- Certain autoimmune disorders
- High cholesterol and blood pressure
- Certain antibiotics, antihistamines, antidepressants and other medications (such as Accutane)
Often, people have multiple risk factors for MGD.
How is MGD detected?
Meibomian gland dysfunction often doesn't have any symptoms until it causes eye dryness. Since its symptoms are nearly the same as those of dry eye syndrome, only an eye doctor can tell for sure if you have MGD.
First, they will ask you some questions about your eye symptoms and health history. Many doctors will also do a standard eye exam as part of the process.
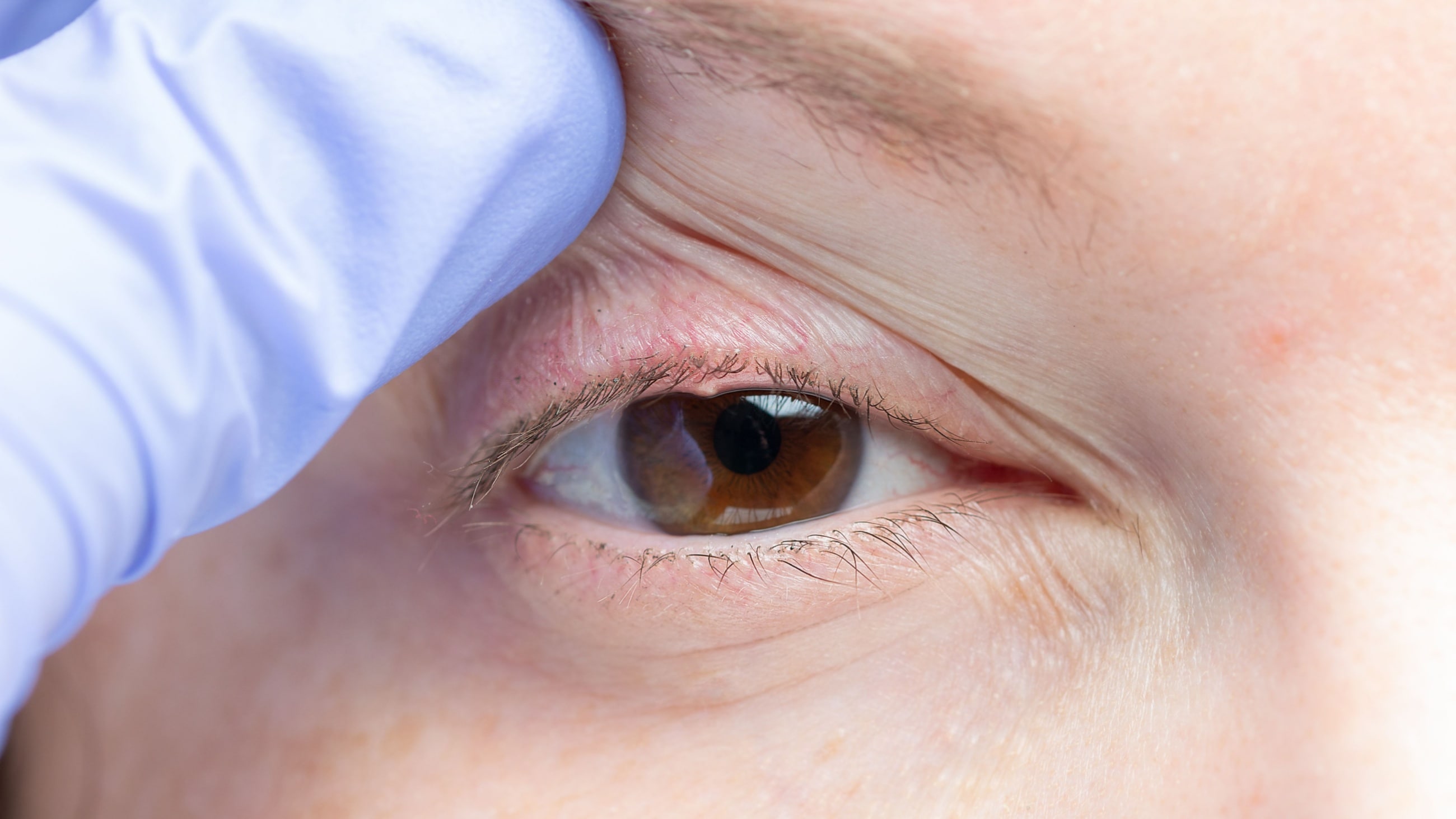
One simple technique your doctor might use to detect MGD is to apply pressure to your eyelid. This is done to express the contents of the meibomian glands. Observing these secretions can often allow an eye doctor to determine if you have meibomian gland dysfunction.
Because meibomian gland dysfunction affects the stability of the tear film, your eye doctor may also test the quality, quantity and stability of your tears.
One common test is called the tear break-up time (TBUT) test. In this simple, painless test, the eye doctor applies a small amount of dye to the front surface of your eye. Then they examine your eye with a cobalt blue light, which causes your dyed tears to glow. This enables them to see how quickly your tear film loses its stability (breaks up) on the surface of your eye.
Another method of TBUT test measures the break-up time with imaging software. This method doesn't require any dye.
Your doctor may also do a Schirmer's test to check the volume of tears in your eyes. They'll place special strips of paper just inside your lower eyelids for a few minutes. They can then measure your tear volume by how many millimeters of the strips are wet.
Other tests your doctor may do include:
- Meibography – Meibomian gland imaging
- Osmolarity – Uses samples or a special viewing device to check tear makeup
- MMP-9 inflammation test – Uses a small tear sample to check for MMP-9 inflammatory molecules commonly found with dry eye disease
- Interferometry – Uses a special viewing device to analyze the lipid layer of tears
SEE ALSO: How to use eye drops without spilling them all over your face
Treatment of meibomian gland dysfunction
Your eye doctor may recommend one or more treatment options for your MGD, starting with:
At-home care
One common treatment for MGD is warm compresses followed by massaging the eyelids. The goal of this treatment is to unclog the openings of the meibomian glands.
Some doctors recommend using a warm, moist washcloth over the closed eyelids. Others recommend using a special eye mask to deliver heat to the eyelids. In either case, the heat therapy is followed by massaging the eyelids to expel the melted oils from the glands.
Eyelid hygiene is also key in at-home care for MGD. Gently clean your eyelid margins once or twice a day using a mild cleanser or baby shampoo. Your eye doctor may recommend a special lid scrub to use as well.
Unfortunately, warm compresses and lid massages often aren't enough to treat meibomian gland dysfunction and eliminate symptoms.
Today, there are many treatment options for MGD. They may be used separately or in combination with each other. Modern treatments for meibomian gland dysfunction include:
LipiFlow
The LipiFlow thermal pulsation system is an in-office treatment for MGD. This device applies heat to the eyelids to melt waxy deposits in the meibomian glands. At the same time, it applies pulsed pressure to the eyelid to open and express the contents of the glands.
The LipiFlow device attaches to the eyelid for the 12-minute treatment session. The system is designed so there is no transfer of heat or pressure from the eyelids to the eyeball itself. Research has shown that one treatment can improve meibomian gland secretions and dry eye symptoms for up to three years.
Systane iLux
The Systane iLux MGD treatment uses a portable, hand-held device. It has an LED heat source to warm the eyelids and melt the clogs inside the meibomian glands.
Once the heat has melted the clogs, your eye doctor will apply compression to the lids to express the meibomian glands. Most patients can be treated with the Systane iLux system in less than eight minutes.
Studies show that iLux treatment results in significant improvements in meibomian gland dysfunction and dry eyes within two to four weeks.
TearCare
TearCare is another in-office treatment for MGD. This system consists of single-use adhesive heating patches applied to the external eyelids. The patches are connected by a cable to a small, reusable handheld heating unit. After the 15-minute heating period, the eye doctor squeezes the lids to open and drain the clogged meibomian glands.
Studies show that TearCare is an effective treatment option for MGD and dry eye disease and can reduce symptoms for six to 12 months.
Intense pulsed light (IPL)
This treatment has been used by dermatologists for years to treat acne rosacea. It is also an effective treatment for meibomian gland dysfunction and dry eye symptoms.
IPL treatment applies intense pulses of visible and infrared light to the eyelids. Each treatment session lasts about 10 minutes. Typically, multiple treatments are scheduled about two weeks apart to produce long-lasting effects.
Intense pulsed light treatments reduce the eyelid inflammation that causes clogged meibomian glands. A three-year study of IPL found 93% of subjects were satisfied with the improvements in their symptoms of meibomian gland dysfunction.
BlephEx
BlephEx is an in-office treatment for blepharitis. But doctors also use it to reduce the symptoms of meibomian gland dysfunction. The hand-held device gently scrubs the eyelid margins with a rotating, medical-grade sponge.
The exfoliating action removes an inflammation-causing biofilm that can form on the eyelids. It is this biofilm that causes the meibomian glands to clog up. The treatment usually takes less than 10 minutes to clean all four eyelids.
Lid debridement
In this treatment, your eye doctor uses a hand-held device to remove keratin and other debris that can adhere to eyelid margins and clog meibomian glands. Lid debridement can relieve dry eye symptoms and improve meibomian gland function.
Antibacterial eye drops
Antibacterial eye drops may help resolve MGD related to demodex mites and blepharitis. During your eye exam, your eye doctor will advise you whether this is a good option for you.
Cyclosporine and other eye drops
Cyclosporine is an agent that modifies the body's immune response in a specific way. This medication can help improve tear film stability and inflammation of the eyelid margins.
Other treatment options that work similarly include:
- Lifitegrast eye drops
- Steroid eye drops
- Acoltremon eye drops
- Varenicline nasal spray
- Serum tears
Oral medication
Your doctor may prescribe oral medication such as doxycycline or azithromycin to treat moderate to severe MGD. Both options are antibiotics with anti-inflammatory and lipid-regulating properties to help improve dry eye symptoms.
Omega-3 supplements
Some eye doctors recommend omega-3 fatty acids to help relieve MGD symptoms. A diet rich in omega-3s may also decrease the risk of future episodes of meibomian gland dysfunction. These fatty acids may help reduce inflammation and lower the risk of buildup within the meibomian glands.
See an eye doctor
Only an eye doctor can tell for sure if you have meibomian gland dysfunction. They can provide the best MGD treatment options for your needs. If you have signs and symptoms of MGD, see an eye doctor to get relief.
READ NEXT: Punctum of the eye