New Device Lets You Test Your Eye Pressure Every Day — At Home
May 2017 — The FDA-approved Icare Home tonometer is now available in the United States for people who need to closely monitor their intraocular pressure (IOP).
IOP can fluctuate significantly throughout the day, making it difficult for eye doctors to prescribe appropriate dosages of glaucoma medication to reduce IOP spikes. High IOP damages the eye's optic nerve, causing permanent vision loss.
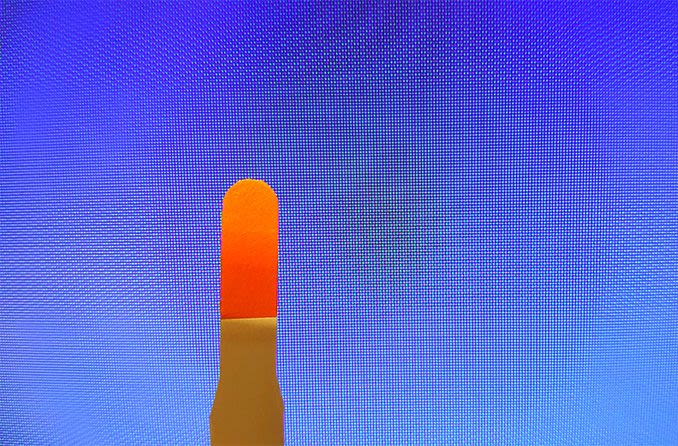
The Icare Home device is easy to use: you just position it over your eye, with the help of red and green light signals. There's no puff of air, no drops are needed, and the device automatically identifies which eye you're measuring.
An automated measuring sequence can take either a single measurement or a series of six measurements, for greater accuracy.
Your eye care professional will download the data with special software and use it to help manage your care. If you are at risk for glaucoma or already have this sight-stealing condition, you may be a candidate to use Icare Home. Your eye doctor can provide details.
Research Says You Should Rethink Your Yoga Routine if You Have Glaucoma
January 2016 — It may seem counterintuitive that a calming exercise like yoga could make your pressure rise, yet that is precisely what was uncovered by researchers at New York Eye and Ear Infirmary of Mount Sinai (NYEE).

To see the four yoga poses that may increase intraocular pressure, please click here.
While yoga practice may benefit the mind and body in many ways, certain poses can put your vision at risk if you have glaucoma. Inverted or head-down positions can cause a dangerous rise in intraocular pressure (IOP).
In this new study, people with healthy eyes and those with glaucoma showed a rise in IOP while performing downward facing dog, standing forward bend, plow, and legs up the wall.
Furthermore, IOP didn't return to its baseline level soon after releasing the pose. Even after a 10-minute wait, the pressure remained slightly elevated in most people.
Elevated IOP is the most common known risk factor for glaucomatous damage, and it often leads to vision loss. So any activity that can cause IOP to rise should be avoided if you have glaucoma.
NYEE research associate and lead author of the study, Jessica Jasien, M.En., suggests that glaucoma patients talk to their yoga instructors about the need to avoid inverted poses so that modifications can be suggested. And keep in mind that even routine poses can be harmful. In fact, in this study, the greatest increase of pressure occurred during downward facing dog, a staple of most yoga routines.
A report of this study appeared in the journal PLOS One in December.
People's Gait May Reveal Whether They Have Glaucoma
October 2015 — For people with glaucoma, walking isn't as easy as it once was. Even in the early stages of the disease, when vision hasn't yet deteriorated noticeably, glaucoma sufferers may walk more slowly, bump into things, stumble and sway.
Researchers at Washington State University School of Electrical Engineering and Computer Science have been using sensors in clinical trials to analyze people's gait. The trials are comparing the gaits of glaucoma patients with those of people in control groups.
The sensors are worn on special shoes and can detect the length and evenness of a step, as well as the equity between the feet. By detecting changes and abnormalities in the way a person walks, the analysis could provide an early indication of glaucoma's presence and could also prevent serious injury from falls.
The University of California, Los Angeles, is recruiting more participants in various stages of glaucoma for the next phase of the research.
Glaucoma Drug and Weight Loss Program Combined to Battle Blinding Disorder
October 2014 — Idiopathic intracranial hypertension (IIH) is a condition that causes increased pressure in the head and eyes. Those who suffer from IIH tend to be young women who are obese, 86 percent of whom develop vision loss due to strain on the optic nerves.

In a study, effective management of IIH symptoms included workouts and healthy diets.
A new study from Saint Louis University looked at the effect glaucoma medication had on patients with IIH-related vision loss when combined with weight loss programs. The trial included 165 participants with IIH who had mild vision loss. They were enrolled in weight loss programs with meal plans, simple workout regimens and consultations with weight loss coaches. Participants were randomly assigned to use either the glaucoma medication or a placebo.
The vision of the participants who received the glaucoma medication improved twice as much as that of the placebo recipients. Additionally, those who used the medication and lost weight were able to complete daily tasks more easily and had increased quality of life.
The next part of the study will observe whether these changes are a long-term solution to managing the symptoms of IIH. Researchers will check in with participants for five years and record whether symptoms reappear when a healthy weight is maintained.
Marijuana Is Not Effective as a Glaucoma Treatment
July 2014 — If you know someone who's using marijuana or other cannabis products to treat the eye disease glaucoma, tell them it's not going to work.
What's worse, if they're using weed instead of prescribed glaucoma medication, they're wasting precious time — they'll likely continue to lose vision, and the loss is irreversible.

As a treatment for glaucoma, marijuana simply doesn't work. If you don't believe us, ask an eye doctor!
For many years the American Academy of Ophthalmology has been reminding people of these facts, yet the popular belief that weed can treat glaucoma stubbornly persists.
This may be just wishful thinking. Or maybe it's due to 1970s studies that reported lowered intraocular pressure for three to four hours after marijuana was administered. The effect was reportedly not enough for long-term management of the vision-stealing disease.
According to an AAO statement released this month, there is "no scientific evidence that marijuana is an effective long-term treatment for glaucoma, particularly when compared to the wide variety of prescription medication and surgical treatments available." In fact, the Academy added, marijuana lowers blood pressure in the body, which could lower blood flow to the optic nerve, leading to loss of vision.
Additional information about glaucoma and marijuana use is on this website.
Study Finds Sleeping With Head Elevated Reduces IOP
June 2014 — Sleeping on a wedge-shaped pillow that elevates the head 20 degrees reduces nighttime intraocular pressure (IOP) and thereby might help control or reduce the risk of glaucoma.
Fifteen people with self-reported glaucoma and 15 without glaucoma were evaluated in a sleep laboratory on two occasions: in one session, they slept lying flat on their backs with no pillow; in the second session, they slept on a wedge-shaped pillow that elevated their head 20 degrees from the surface of the bed.

Sleeping with your head elevated may reduce your eye pressure at night and decrease your risk of glaucoma-related vision problems.
Baseline eye pressure was measured prior to sleep, then at two-hour intervals during a sleep period lasting six hours.
IOP did not differ significantly between the two positions during the initial (awake) measurement for either group. But during the sleep period, the mean IOP reading when subjects slept on the wedge pillow with their head raised was 1.56 mm Hg lower in the glaucoma group and 1.47 mm Hg lower in the normal group, compared with sleeping flat on the bed.
This corresponds to a 9.3 percent reduction of IOP in the glaucoma group and an 8.7 percent reduction of IOP in the non-glaucoma group, compared with measurements taken when subjects slept on their backs without the pillow.
A total of 25 of the 30 subjects (83.3 percent) had lower eye pressure when sleeping with their head elevated, and 11 subjects (36.7 percent) had reductions in mean IOP that exceeded 10 percent when sleeping on the wedge pillow.
The study authors concluded that sleeping with the head elevated 20 degrees reduces nighttime IOP measurements in glaucoma and non-glaucoma subjects alike, compared with sleeping in the supine position with a flat back.
Researchers at State University of New York Downstate Medical Center in Brooklyn, N.Y. conducted the study; a report of the study appeared in this month's issue of Journal of Glaucoma.
Low Vitamin D Might Be Risk Factor for Glaucoma
April 2014 — Low blood levels of vitamin D could increase your risk of glaucoma, according to a new study.

Spending some time in the sun is the best way to boost your blood levels of vitamin D — and possibly decrease your risk of glaucoma.
In research published this month in Public Health Nutrition, investigators examined the relationship between five categories of serum vitamin D levels and the prevalence of open-angle glaucoma among 6,094 adults in South Korea.
The odds ratio of having glaucoma among study participants comprising the group with the lowest vitamin D levels was significantly higher than that for those with more robust vitamin D levels.
The researchers also found that predictors for worsening of open-angle glaucoma — such as high eye pressure and changes in appearance of the optic nerve
— had a significant relationship with low serum vitamin D levels.
The study authors concluded that vitamin D deficiency should be considered a potential risk factor for the development of open-angle glaucoma.
Sleeping on One Side May Worsen Glaucoma
January 2014 — A new study from South Korea that examined the sleeping habits of people with glaucoma found that people sleeping on just one side were more likely to sleep with the affected eye facing downward.

The researchers say that position raises the eye's internal pressure and may accelerate the deterioration of the eye. In glaucoma, the optic nerve is often damaged by increased intraocular pressure, which causes tunnel vision and eventual blindness.
The study, conducted by the Department of Ophthalmology at the Chungnam National University hospital, studied the sleeping habits of 430 glaucoma patients who had a visual field loss that was worse in one eye. They found 132 of the patients preferred to sleep on one side. Of these patients, 67 percent usually slept with the worse eye downward.
The researchers also compared the sleeping habits of glaucoma patients with elevated intraocular pressure with those with normal pressure. Approximately 66 percent of the patients with normal-tension glaucoma preferred to sleep with the worse eye downward, and 71 percent of the patients with high-tension glaucoma slept that way.
While the results don't prove that sleeping position accounts for worsening glaucoma on one side, the researchers believe they at least verify a link between the preferred sleeping position and asymmetric visual field loss between the eyes.
Likelihood of Blindness From Glaucoma Has Dropped by Nearly Half
January 2014 — The probability of blindness due to the serious eye disease glaucoma has decreased by nearly half since 1980, according to a study conducted by the Mayo Clinic. The study was the first to assess long-term changes in the risk of progression to blindness and the population incidence of glaucoma-related blindness.

"Puff tests" and other testing for glaucoma have become almost routine during eye exams. Early detection of the disease helps explain why the probability of blindness has decreased, at least in some areas.
Researchers analyzed the medical records of all the people 40 and older in Olmsted County, Minn., who were diagnosed with the eye disease between 1981 and 2000. They compared these people with patients diagnosed with glaucoma between 1965 and 1980.
The incidence of glaucoma did not change, but the risk of going blind in at least one eye fell from about 26 percent in the earlier group to less than 14 percent in the newer group. The researchers also found that the annual incidence of glaucoma-caused blindness dropped by more than half.
Advances in diagnosis and therapy are likely causes for the decrease, according to researchers. But they caution that a significant proportion of glaucoma patients still progress to blindness. Glaucoma is a leading cause of irreversible blindness worldwide and affects more than 2.7 million individuals aged 40 and older in the United States and 60.5 million people globally.
READ NEXT: Hypotony: Low Eye Pressure