Corneal scarring: Causes, symptoms, treatment and healing time
What is a corneal scar?
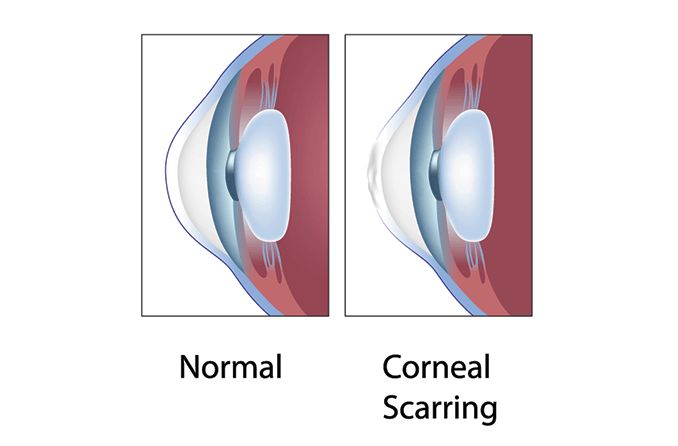
A corneal scar blocks or distorts light as it enters the eye and can lead to decreased vision. Corneal scars are most commonly caused by an infection, injury or disease; however, procedures such as an eyelash lift and laser eye surgery also pose a slight risk.
The cornea is the clear front surface of the eye. It has five layers, listed from outermost to innermost:
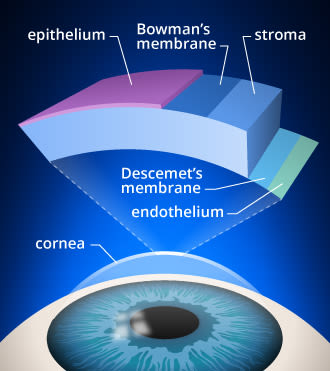
Layers of the cornea. Corneal cross-linking strengthens bonds in the stroma of the cornea, which is the layer from which tissue is removed during LASIK surgery.
Epithelium
Bowman’s layer
Stroma
Descemet’s membrane
Endothelium
The cornea helps you see clearly by bending light onto the lens and retina as the light enters your eye. The outer layer of the cornea (the epithelium) also helps protect your eyes from irritants such as dirt, dust and germs.
What causes corneal scarring?
Anything that can damage the cornea has the potential to cause corneal scarring, including:
Corneal abrasion (scratch) or eye injury – Most of the time, a scratch on the cornea is a minor injury that only damages the outer layer, making it less likely to scar. More serious injuries caused by a hard hit to the eye or an abrasion from something sharp are more likely to result in a deeper wound and a corneal scar.
Eyelash lift – This is a cosmetic treatment that makes your eyelashes look fuller and curlier. A special perming solution is used to achieve these effects. Corneal scarring is possible if the solution gets in your eyes.
PRK (photorefractive keratectomy) – PRK is a surgery that uses lasers to correct nearsightedness, farsightedness and astigmatism by changing the shape of the cornea. Like any surgery, there are risks to having PRK, and corneal scarring is one of those risks.
Conditions that can cause corneal scarring
Not all corneal scarring results from injury or trauma. Some eye conditions can also cause corneal scarring, including:
Corneal dystrophies – These are eye diseases that involve changes in the cornea, and they are often hereditary. Some cause blindness and eye pain, while others don’t have any noticeable symptoms. Most corneal dystrophies get worse over time. Examples include:
Fuchs’ dystrophy – Fuchs’ dystrophy is when the endothelium layer is damaged and can’t efficiently pump excess fluid out of the stroma. This causes the cornea to swell and change shape, resulting in hazy vision and light sensitivity. It usually affects both eyes.
Reis bucklers corneal dystrophy – This disorder affects the epithelium and Bowman’s layer at the front of the cornea, causing scarring and clouding of Bowman’s membrane. People with Reis bucklers corneal dystrophy will have blurry vision or double vision in one eye.
Keratoconjunctivitis – This is inflammation that affects the eyes’ superficial cornea and conjunctiva (the loose connective tissue that covers the front of the eyeball). Keratoconjunctivitis can be caused by a virus, autoimmune disorder, bacteria, or allergies. Although rare, some forms of keratoconjunctivitis can result in corneal scarring.
Newborn conjunctivitis – Also known as ophthalmia neonatorum, this condition occurs within a baby’s first 30 days of life. Caused by a chlamydial, bacterial or viral infection, it can result in corneal scarring in both eyes and potentially even blindness.
Stevens-Johnson syndrome (SJS) – This syndrome causes painful blisters and lesions on the skin and mucous membranes and can lead to serious eye problems. Complications of severe eye disease include conjunctival and corneal scarring. The most common cause of SJS is an allergic reaction to a medication, though it can also result from an infection.
Xerophthalmia – A group of eye issues caused by vitamin A deficiency, it’s characterized by extreme dry eye and night blindness. It mostly affects infants and young children in poverty-stricken regions around the world.
Trachoma – Trachoma is a serious bacterial infection that can be transmitted through bodily fluids or contact with an infected person’s mouth, nose or eyes. It can result in corneal inflammation and cause the eyelashes to turn in. This can lead to repeated corneal abrasions and eventual scarring. Though uncommon in the U.S., trachoma is the No. 1 infectious cause of preventable blindness in the world.
Developmental glaucoma – This type of glaucoma affects babies, children and teenagers. There is an additional risk for corneal scarring or opacification because children’s eyes are still pliable and soft, and their high intraocular pressure can stretch and enlarge the cornea and other parts of the eye.
Keratoconus – People with this eye disorder have abnormal thinning of the cornea, which causes the front surface of the eye to bulge forward. Corneal scarring can occur when the overly thin cornea has been subjected to excessive eye rubbing or extended contact lens wear.
SEE RELATED: Apert syndrome
What are symptoms of corneal scarring?
A scar on the cornea can affect your vision, making it hard for you to see clearly. Symptoms of a corneal scar include:
Hazy or cloudy vision
Very red, watery eyes
How is corneal scarring diagnosed?
Corneal scars have the appearance of white opaque spots on the cornea. Some are visible without any specialized equipment, while others are more difficult to detect. Your eye doctor can use certain tests and equipment to help determine if you have a corneal scar:
Slit-lamp exam – A slit lamp is a microscope with a bright light attached that your eye doctor uses to see your cornea clearly.
Corneal topography scan – This scan shows any abnormalities including scarring and other conditions that may affect the health of your cornea.
Visual acuity test – In an acuity test, you read letters on a wall chart at a distance to test the clarity and strength of your central vision. If you have trouble reading the letters, that may be a sign of a corneal scar.
Can a corneal scar heal on its own?
Minor corneal scratches and other superficial injuries can heal on their own (without resulting in permanent scarring), usually in one to two days. Your eye doctor may prescribe oral tetracyclines, topical steroids or eye drops to reduce inflammation and help you heal properly.
If the deeper layers of the cornea become damaged due to an injury or infection, a scar may form that can cause a loss of transparency (also called corneal opacity).
If you have corneal scarring that affects your eyes or how you see, you may need some form of treatment.
How is corneal scarring treated?
Treatment for a corneal scar typically depends on how seriously a patient’s vision is affected and how deeply the cornea is scarred. The underlying cause is taken into consideration so future scarring can be prevented. Treatment options include:
Vision correction – If a corneal scar makes your vision blurry or cloudy, prescription glasses or rigid gas permeable (RGP) contact lenses may make it easier for you to see clearly.
Laser surgery – Small amounts of scar tissue and shallow scars can be removed with laser treatment known as PTK (phototherapeutic keratectomy).
Corneal transplant – If contact lenses or laser treatments don’t work, you may need cornea transplant surgery (keratoplasty). During a corneal transplant, a surgeon replaces a patient’s scarred cornea tissue with an organ donor’s healthy corneal tissue.
READ NEXT: Corneal disease
Corneal opacity (scar). Kellogg Eye Center University of Michigan Health System. December 2014.
Corneal disease. Cleveland Clinic. August 2020.
Corneal scar. Kaiser Permanente Permanente Medicine. Accessed March 2020.
Unraveling the mysteries of corneal scarring. Cleveland Clinic. November 2014.
Corneal conditions. National Eye Institute. August 2019.
Corneal dystrophies. National Eye Institute. June 2019.
Control of scar tissue formation in the cornea: strategies in clinical and corneal tissue engineering. Journal of Functional Biomaterials. September 2012.
Stevens-Johnson syndrome. Johns Hopkins Medicine Wilmer Eye Institute. Accessed March 2022.
Xerophthalmia. EyeWiki. March 2022.
Hygiene-related diseases: Trachoma. Centers for Disease Control and Prevention. November 2021.
Childhood glaucoma. Glaucoma Research Foundation. 2016.
Keratoconus. MedlinePlus. August 2020.
Corneal topography. American Academy of Ophthalmology. May 2021.
The ins and outs of corneal wound healing. Review of Optometry. April 2016.
No insult to injury: treating corneal trauma. Review of Optometry. April 2016.
About corneal transplantation. American Academy of Ophthalmology. September 2021.
Page published on Wednesday, April 20, 2022
Page updated on Tuesday, April 19, 2022
Medically reviewed on Tuesday, March 29, 2022






