Posterior subcapsular cataract: Description and causes
What is a posterior subcapsular cataract?
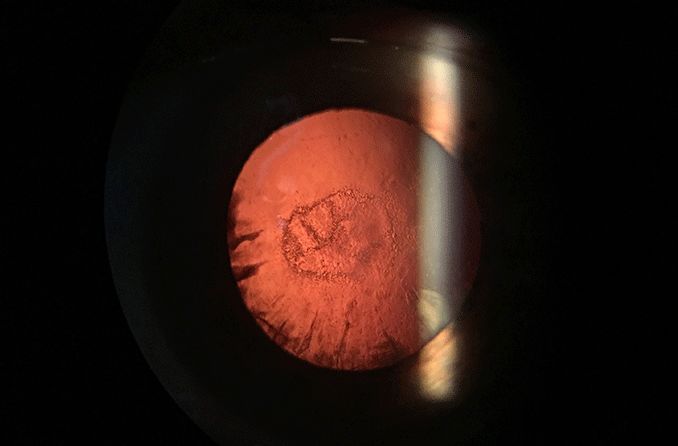
Posterior subcapsular cataract (PSC) is a fast-growing opacity in the rear of the natural lens. This cataract is most common in people who take steroids or have diabetes. PSC symptoms can develop over a few months. They include light sensitivity, glare and decreased vision, especially at near.
A wide variety of medical conditions and risk factors contribute to the formation of PSC. Due to this, PSC occurs in younger people more often than other types of cataracts.
PSC is the least prevalent of the three common types of cataracts. According to the Beaver Dam Eye Study, the incidence of PSC was about 3% in one eye. The incidence of cortical cataracts was about 8%, and nuclear cataracts was about 13%.
What causes posterior subcapsular cataracts?
PSC is caused by the buildup and clumping of protein fibers in the back of the lens, just in front of the posterior lens capsule. This clumping of proteins disrupts the transparency of the lens fibers, resulting in opacities in the lens. Quality of vision decreases because light rays are scattered, and fewer light rays reach the retina.
The process of lens protein buildup and clumping occurs naturally with aging. Other factors that can contribute to the development of PSC include:
Long-term use of corticosteroids
Medical conditions such as diabetes
Ocular conditions such as inflammation from uveitis, retinitis pigmentosa, trauma and radiation exposure
Certain skin disorders such as atopic dermatitis
High amounts of exposure to UV radiation
How are posterior subcapsular cataracts classified?
Your doctor may tell you that you have a 1+ to 3+ PSC. This is a classification system that grades the cataract according to size, in millimeters:
PSC 1+ – 1 mm to 2 mm
PSC 2+ – 2 mm to 3 mm
PSC 3+ – 3+ mm
PSC is a fast-growing cataract that can progress fairly quickly from PSC 1+ to PSC 3+. Your doctor will monitor the PSC and recommend the appropriate management, including surgery.
What are the symptoms of posterior subcapsular cataracts?
A PSC limits and scatters the light that reaches the retina, causing visual disturbances. Symptoms from PSC develop quickly as the PSC grows, and include:
Decreased vision, with near vision worse than distance vision
Sensitivity to bright lights
Glare, especially from headlights when driving at night
What is the treatment for posterior subcapsular cataract?
The treatment for a posterior subcapsular cataract is cataract surgery. It is a common surgery and carries low risk. The surgeon removes the cloudy natural lens and replaces it with a clear artificial lens called an intraocular lens (IOL). The surgery takes about 15 minutes, and you will be able to go home that day.
What can I do to prevent posterior subcapsular cataract?
Your doctor can help you manage conditions such as diabetes or ocular inflammation and trauma that can be risk factors for developing a PSC.
Some additional steps that you can take to decrease your chances of developing a PSC are:
Increase vitamin C, D and E intake with supplements and a diet of fruits and vegetables.
Decrease alcohol consumption.
Minimize UV exposure.
Avoid obesity by maintaining a healthy weight.
Stop smoking.
What does it mean if I have been told I have a posterior subcapsular cataract?
A posterior subcapsular cataract usually progresses quickly. If you are experiencing difficulty with blurry vision and glare while driving, talk to your doctor. They can help you to make an informed decision about your cataract surgery options.
Cataract. American Academy of Ophthalmology. EyeWiki. April 2020.
Incidence of age-related cataract: The Beaver Dam eye study. Archives of Ophthalmology. February 1998.
Risk factors for nuclear, cortical and posterior subcapsular cataracts in the Chinese population of Singapore: the Tanjong Pagar Survey. British Journal of Ophthalmology. August 2003.
Posterior capsule opacification in eyes with steroid-induced cataracts: Comparison of early results. Journal of Cataract & Refractive Surgery. January 2011.
Diabetes, cardiovascular disease, selected cardiovascular disease risk factors, and the 5-year incidence of age-related cataract and progression of lens opacities: The Beaver Dam eye study. American Journal of Ophthalmology. December 1998.
Ocular inflammation in anterior segment. Ocular Therapeutics. May 2008.
Ocular health assessment.Clinical Procedures in Primary Eye Care. Elsevier ScienceDirect. 2007.
Risk factors for posterior subcapsular cataract in retinitis pigmentosa. Investigative Ophthalmology and Visual Science. May 2017.
Anterior segment. Case Reviews in Ophthalmology. Elsevier ScienceDirect. 2018.
The ageing lens and classification of cataracts. Cataract. Elsevier ScienceDirect. 2008.
Contribution of the nurses’ health study to the epidemiology of cataract, age-related macular degeneration, and glaucoma. American Journal of Public Health. September 2016.
Early lens changes seen in patients with atopic dermatitis applying image analysis processing of Scheimpflug and specular microscopic images. Ophthalmologica. 1998.
Vitamin C is associated with reduced risk of cataract in a Mediterranean population. The Journal of Nutrition. June 2002.
Vitamin D deficiency and posterior subcapsular cataract. Clinical Ophthalmology. June 2015.
Etiology of posterior subcapsular cataracts based on a review of risk factors including aging, diabetes, and ionizing radiation. International Journal of Radiation Biology. September 2020.
Cigarette smoking and lens opacities: The Beaver Dam eye study. American Journal of Preventive Medicine. January 1993.
Page published on Friday, September 10, 2021






